- Research
- Open access
- Published:
Cost and economic evidence for asset-based approaches to health improvement and their evaluation methods: a systematic review
BMC Public Health volume 24, Article number: 814 (2024)
Abstract
Background
Asset-based approaches (ABAs) tackle health inequalities by empowering people in more disadvantaged communities, or targeted populations, to better utilise pre-existing local community-based resources. Using existing resources supports individuals to better manage their own health and its determinants, potentially at low cost. Targeting individuals disengaged with traditional service delivery methods offers further potential for meaningful cost-savings, since these people often require costly care. Thus, improving prevention, and management, of ill-health in these groups may have considerable cost implications.
Aim
To systematically review the extent of current cost and economic evidence on ABAs, and methods used to develop it.
Methods
Search strategy terms encompassed: i) costing; ii) intervention detail; and iii) locality. Databases searched: Medline, CENTRAL and Wed of Science. Researchers screened 9,116 articles. Risk of bias was assessed using the Critical Appraisal Skills Programme (CASP) tool. Narrative synthesis summarised findings.
Results
Twelve papers met inclusion criteria, representing eleven different ABAs. Within studies, methods varied widely, not only in design and comparators, but also in terms of included costs and outcome measures. Studies suggested economic efficiency, but lack of suitable comparators made more definitive conclusions difficult.
Conclusion
Economic evidence around ABAs is limited. ABAs may be a promising way to engage underserved or minority groups, that may have lower net costs compared to alternative health and wellbeing improvement approaches. ABAs, an example of embedded services, suffer in the context of economic evaluation, which typically consider services as mutually exclusive alternatives. Economics of the surrounding services, mechanisms of information sharing, and collaboration underpin the success of assets and ABAs. The economic evidence, and evaluations in general, would benefit from increased context and detail to help ensure more nuanced and sophisticated understanding of the economics of ABAs. Further evidence is needed to reach conclusions about cost-effectiveness of ABAs.
Background
Asset based approaches to health
In the United Kingdom (UK) a growing and ageing population, and increasing burden on health services, is leading to an emphasis on prevention, integration of services and supporting people to manage their own health [1]. Historically, approaches to improve population health have utilised a ‘deficit model’: focusing on identifying the problems and needs of the population that require costly curative services [2,3,4]. This undermines the role that individuals and communities can play as active participants to create, acquire and maintain their own health [2]. The NHS Long Term Plan (2019) calls for a shift towards a pro-active model for health and well-being, whereby society values and tries to enable a state of complete physical, mental and social well-being, as opposed to waiting for individuals to reach ill-health before receiving support and treatment [5, 6]. This recognising that positive health and social outcomes can be achieved more successfully and efficiently if there is a shift away from a ‘doing to’ culture (whereby individuals are treated once they become unwell) to one that respects meaningful and ‘preventative’ social change (where individuals are supported and empowered to make healthier choices, promoting continued good health) [7].
‘Assets’ and ‘asset-based approaches’ (ABAs) aim to identify and utilise health promoting or protective factors that are most likely to lead to higher degrees of overall health and wellbeing, achievement, and sustainability [2]. ‘Assets’ are community resources, and can refer to financial resources, physical infrastructure, facets of social capital or individual capabilities [8]. Assets operate across multiple levels, for example enabling self-esteem and resilience at the individual-level, supportive friendship and peer networks at community-level, and provision of positive environmental and organisational resources to promote health and well-being at structural-levels [9]. ABAs build on the skills of local people, the power of local associations and the supportive functions of institutions and services, to build stronger, more sustainable communities [10]. ABAs are considered a subset of community-based interventions, distinctly implementing interventions which aim to build capacity, engagement, knowledge and/or resources within a defined community asset e.g., local churches, existing community groups, local parks or hyperlocal geographical areas. They make visible and value the skills, knowledge, connections and potential in a community [11].
Generally speaking, health and wellbeing services suffer from disparity in uptake and provision, such that uptake is socially patterned, and services are more likely to be successfully accessed by affluent groups—termed the ‘inverse prevention law’ [12, 13]. Therefore, preventative health interventions may not reach the most disadvantaged and those furthest from reaching their full health potential [12]. Consequentially, preventative services may benefit from ABAs. One of the main advantage of ABAs, beyond standard community interventions, is that they can engage: i) members of society who are more likely to be disengaged with traditional methods of service delivery; and ii) specific populations (e.g. cancer survivors). They do this by tapping into existing community networks, making use of existing rapport and trusted connections, to facilitate health-related conversations and information sharing which otherwise may not occur. Therefore, equitable community-based development may be best supported through ABAs [14, 15]. Further, building on existing assets potentially reduces high-level start-up costs, such as reducing the need for highly trained staff to address participant care needs, alongside delivering engagement and implementing strategies. In ABAs, individuals working in established groups are typically already well-versed at meeting their participants’ needs [16]. Since there are reduced start-up costs, and engagement is expected to be high, from an economic perspective, ABAs offer a potentially efficient approach to delivering benefits for participants.
Economic evaluation of ABAs
Decision-makers must routinely make choices about how to prioritise public health problems and related interventions within limited budgets and resources. In making such choices, decision-makers can benefit by knowing the financial resources required to implement each intervention and how money invested compares to outcomes achieved [17]. Economic comparisons are challenging in the context of: i) comparing one ABA to another ABA; and ii) comparing ABAs to other types of health and social care interventions. To date, it is unclear what economic evidence has been collected in the context of ABAs and what methods have been used to generate this evidence.
Well-established frameworks, known as economic evaluations (EEs), inform decision-makers about the comparative costs and outcomes (or ‘benefits’) of a range of mutually exclusive courses of action for health and social care. From this definition, it is worth emphasising that EEs do not exclusively focus on costs—outcomes/benefits are crucially important too. Typically, EEs involve exploring which option will maximise health and social care outcomes, most commonly in the form of quality-adjusted life years (QALYs) that seek to capture impacts on life extension and its quality, subject to the constraints of the health sector budget. Public health and social care interventions, including ABAs, may be considered complex interventions, in that they offer flexibility in intervention delivery and individual-level variability in outcomes (e.g. improving choice, access and participation in healthcare, education, housing, employment, social activity and personal care) [18]. Complex intervention research “goes beyond asking whether an intervention works in the sense of achieving its intended outcome – to asking a broader range of questions (e.g., identifying what other impact it has… taking account of how it interacts with the context in which it is implemented, how it contributes to system change…)” (P.1, [19]). Therefore, while EEs may be appropriate to assess the value of ABAs, the use of health-focused outcomes, such as QALYs, are unlikely to capture their full impacts. Wider wellbeing outcomes, often measured as wellbeing adjusted life years (WALYs or WELBYs), have received growing interest in the evaluation of public health interventions [20, 21]. While these measures purport to measure and value a broader range of dimensions of health and wellbeing, they are generally viewed as sub-optimal for evaluating complex interventions where the full spectrum of benefits extends well beyond health [22].
Beyond outcome measurement, the EE techniques that typically utilise QALYs (e.g. cost-utility analyses) generally focus on the health care sector (health perspective), often again ‘missing’ some of the important wider societal impacts. A wider societal perspective may be adopted, capturing costs across sectors (e.g. beyond health) with the aim of maximising welfare gain to society [23]. However, this approach is still limited, with impact primarily affecting the ‘cost side’ of the equation. EEs which seek to capture the full range of health and non-health costs and benefits across different sectors (e.g. cost consequence analysis, cost benefit analysis or multicriteria decision analysis) may be more relevant in this context. However, these approaches require multidimensional datasets, potentially complex modelling approaches, and offer an opportunity for inappropriate interpretation of results if the evaluation is not appropriately designed for the decision context [24].
Importantly, health equity, a key objective in public health policy, is rarely captured in economic evaluations [25]. With the increasing awareness of inequity in health improvement, it is essential that health economic methodologies develop to capture this under-reported outcome. Health economics is regularly centred in the quasi-egalitarian value judgement that ‘a QALY is a QALY’; where “QALYs are equally weighted and the health outcome is worth the same no matter how it is achieved, or by whom it accrues” (P.231, [25]). This assumption conflicts with an increasing focus on improving health equity and reaching under-served populations. As ABAs seek to reach those furthest from their health potential, there is opportunity for intervention impact to be greater than it would be for the general population. Specifically in the context of prevention, health improving behavioural shifts (e.g. increased use of health services) may be more impactful when initial behaviours were more harmful (i.e. those who rarely access services may see greater health and wellbeing improvements than those who already regularly engage with services). More broadly, the formerly prevalent view of health gain maximisation – where the objective is primarily to maximise total health benefit [26, 27] – may be undervaluing some interventions as it does not capture the entire impact and value of engaging disengaged individuals to effectively manage their own health. Thus, one might question the applicability of non-targeted health maximising of QALYs in the community care setting – perhaps it does matter by whom it is accrued, providing an argument for weighting cost per QALY by who is benefitting. Additionally, others have noted that allocation of health care resources solely based on health maximation can lead to discrimination against certain groups [28].
A challenge in evaluating ABAs is establishing a suitable alternative to compare the ABA to. In the case of novel asset-based interventions, which are unique in their localised social structures, appropriate comparators are not always clear. The intervention may be compared to the ‘absence of the intervention’ and/ or ‘standard care’. However collecting data for these alternatives is challenging with ABA interventions, since they often involve whole communities in a specific locale (e.g. potential lack of unaffected ‘control’ individuals) and often utilise information sharing and capacity building (consequently statistical ‘contamination’ is likely between intervention and control groups—discussed further later). Absence of a suitable alternative precludes a full EE, and more generally can make it difficult to robustly determine the impact of an intervention.
To better support development and evaluation in complex intervention settings, the National Institute of Health Research and the UK Medical Research Council Guidance commissioned a framework [originally developed 2006; last updated 2021] [19]. This guidance is well positioned for ABA development as it recognises the context specific complexity, framing interventions as events in a wider system. The framework appreciates the pragmatic embedding of services, and its conflict with the assumptions of mutual exclusivity of interventions required for current EE methods – suggesting supporting qualitative studies may be useful to support interpretation of EEs [19]. The framework highlights crucial aspects of evaluation design, including appropriate: comparator; choice of outcome measure or evidence of change; study design; and, costs (including implementation and set-up costs) [19].
Recent developments in the guidance have focused on giving attention to properties of the intervention itself, such as: range of behaviours targeted; expertise and skills required by those delivering and receiving the intervention; number of groups; community setting; and, level of flexibility of the intervention or its components. Appropriate design of complex interventions allows for flexibility in implementation, whilst maintaining the integrity of the core intervention components. This recognises that the ‘same’ ABA applied in two different settings may look different as they appropriately and intentionally adapt to the community setting and target demographic needs. These flexible properties of the intervention have implications for many aspects of its evaluation, and subsequent interpretation. Thus, intervention detail will be considered within this review.
Aims
To make best use of scarce public budgets, it is important to understand the current cost and economic evidence base for ABAs. Further, to inform future research, we want to investigate the methods used to create the current evidence. Thus, this systematic review seeks to address:
-
i)
What designs, methods, and outcomes measures have been used to produce cost and economic evidence?
-
ii)
What is the accrued evidence for the cost and economic impact of ABAs?
Methods
The protocol for this systematic review has been registered in PROSPERO (CRD42021236548). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed [29].
Patient and public involvement (PPI) and stakeholder contribution
Given the broad array of potential community assets, and the flexibility of ABAs, it is challenging to outline a formal or universal definition. Hence, PPI partners and stakeholders were closely involved in defining and categorising ABAs, development, and finalisation of the search terms and strategy, and evaluating the quality of evidence found (e.g., reflecting on the range of outcome measures used and their suitability). They brought specific experience to the review through their roles as a local authority commissioning manager and local Healthwatch co-production facilitator [‘Healthwatch’ is a health and social care champion in England, which ensures service providers and decisions makers listen to public feedback, with the aim to improve care (https://www.healthwatch.co.uk/)]. Each was familiar with ABAs prior to involvement in this study. This level of partner involvement was essential in the exploratory work to help ensure the questions asked of the literature and focus of analysis resonated with public health practice.
Search strategy
The search strategy consisted of three broad components capturing terms associated with: i) costing; ii) intervention detail; and iii) locality. The search strategy was developed with PPI contribution (outlined in Sect. "Inclusion and exclusion criteria"). The second component (intervention detail) received careful attention, helping to ensure eligible papers where the intervention was not explicitly termed or identified as an ABA were captured. Terms included: ‘asset’; 'coproduction’; ‘community development’; ‘capabilities’; ‘resilience’; ‘salutogenesis’; ‘self-care’; ‘participatory approach’; ‘peer support’; ‘intervention’; ‘social prescription’; ‘health promotion’; ‘lay worker’; ‘wellbeing officer’; ‘community health worker’; ‘capacity’; and ‘upskill’. Complete search terms are given in Supplementary Material 1.
Electronic bibliographic databases [MEDLINE (via PubMED); Cochrane Centre Register of Controlled Trials (CENTRAL); and Web of Science] were searched on 07.03.23, with no publication date restrictions.
Inclusion and exclusion criteria
The following inclusion and exclusion criteria were employed.
Inclusion – all required:
-
Interventions categorised as ABA (following our above definition), even when not explicitly named or labelled as such.
-
Studies which evaluated the ‘cost’, or ‘costs and benefits’ relating to at least one ABA.
-
Interventions delivered by non-clinical professionals – e.g. community members, community service staff. Interventions may involve a training component, supportive role or be co-produced with health practitioners.
-
Peer reviewed papers only.
-
English language only.
Exclusion, where any of the following apply:
-
Interventions delivered in clinical settings (i.e. interventions centred in hospital or General Practices).
-
Community setting not detailed.
-
Interventions administered via telephone or cyber communication, unbound by geographical constraint.
-
Interventions delivered exclusively by a clinical professional.
-
Studies which do not report cost(s) associated with the intervention.
Study selection
Database search results were extracted to a citation manager (Endnote X9) where duplicates were identified and removed. Study details (including title and abstracts) were uploaded to web-based software Rayyan (https://www.rayyan.ai/) for screening. Article abstracts were shared between two researchers (AW & LB). Within Rayyan, each reviewer recorded for each article whether it was rejected or put forward for stage two review.
Articles selected for full-text review were independently compared to the inclusion/ exclusion criteria by two reviewers (AW & LB) to finally determine their inclusion. Where these reviewers disagreed, a third reviewer (JAW) arbitrated.
Data extraction
A data extraction table was developed in MS Excel (Supplementary Material 2), capturing 20 study characteristics, and populated by AW.
Included studies were categorised into three groups:
-
i)
Reporting only implementation and running costs (IRC);
-
ii)
Reporting implementation and running costs AND health and/or social care related costs (IRHSC);
-
iii)
Including an economic evaluation (EE) (thus a joint comparison of costs and benefits comparing the ABA to suitable comparator).
Studies categorised to i) IRC and ii) IRHSC did not require a study comparator.
Quality of reporting assessment
The Critical Appraisal Skills Programme (CASP) quality appraisal tool (reported in full in Supplementary Material 3) was used to assess the risk of bias. CASP was selected as it can be used to assess a wide range of both qualitative and quantitative studies, including, randomised controlled trials, cohort studies and economic evaluations [30]. For each study, a CASP checklist relevant to its study type was selected.
Results
Literature search and evaluation for study inclusion
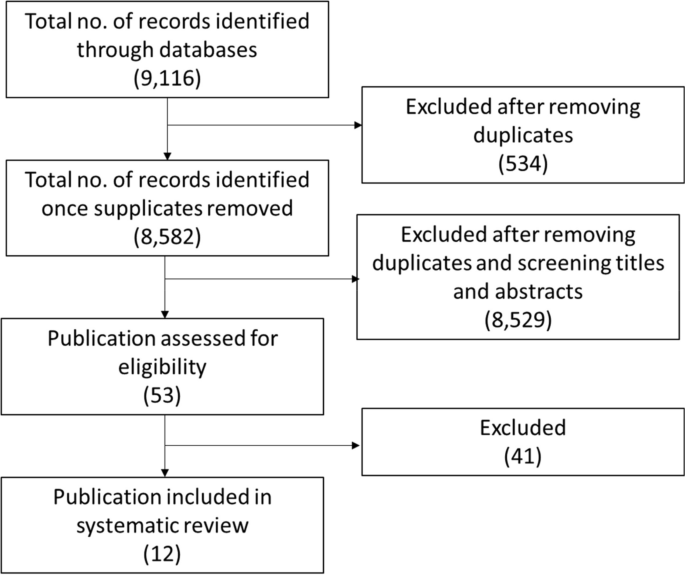
A summary of the process of review and selection is given in the PRISMA flow diagram (Fig. 1).
Searches yielded a total of 9,116 results, of which 534 were identified as duplicates. Subsequently, 8,582 abstracts were screened. Of the screened abstracts, 8,529 studies were excluded, with unanimous (100%) agreement between primary reviewers (AW & LB). The 53 remaining papers underwent full text review: 48 had their inclusion/exclusion status agreed between by the first two reviewers (AW & LB), with disagreement on the remaining five studies resolved by the third reviewer (JAW). Twelve publications were agreed for inclusion.
Studies were appraised using the CASP tools relevant to study type (Tables 1, 2 and 3).
Overview of studies
Twelve papers, representing eleven different ABAs, met the inclusion criteria: Pizzi 2014 [37] assesses the cost-effectiveness of the ABA reported in Gitlin 2012 [36]. Characteristics of included studies relate to the 11 ABAs, treating Pizzi 2014 and Gitlin 2012 as one study.
Most papers [n = 10] were published between 2010–2020, with two published in 2001–2002 [31, 40]. Papers were categorised to: reporting only implementation and running costs (IRC) [n = 1: [36]]; reporting implementation and running costs AND health and/or social care related costs (IRHSC) [n = 2: [32, 34]]; and including an economic evaluation (EE) [n = 9: [31, 33, 35, 37,38,39,40,41,42]]. Here forward, where counted, paper categories are indicated with subscripts.
The reported ABAs were delivered in the: USA [n = 7: nIRC = 1 [36], nIRHSC = 1 [32], nEE = 5 [31, 35, 37,38,39]]; Australia [nEE = 1 [33]]; and the UK [n = 4: nIRHSC = 1 [34], nEE = 3 [40,41,42]]. Among selected studies, only one labelled its intervention as an ABA [42], with others using phrases such as “delivered through community-based organisations” (P.2, [36]) and “engage with social networks and build social capital to enable community ownership” (P.104, [33]). Table 4 details phrases used to describe the ABAs among included papers.
The ABAs included: peer support services [n = 2: nIRHSC = 1 [34], nEE = 1 [41]]; signposting services [nEE = 1 [42]]; educational programmes without a screening component [n = 6: nIRHSC = 1 [32], nEE = 5 [31, 33, 35, 39, 40]]; and educational programmes with a screening component [n=2: nIRC = 1 [36], nEE = 1 [37]]. ABAs were delivered by: upskilled staff from within an existing asset [n = 4: nIRC = 1 [36], nIRHSC = 1 [32], nEE = 2 [35, 37]]; training public members associated with the asset [nEE = 5 [31, 39,40,41,42]]; introducing skilled workers to the asset [n = 2: nIRHSC = 1 [34], nEE = 1 [33]]; and by connecting members from across the community network [nEE = 1 [38]].
Each ABA was run across multiple community sites. Approaches included non-religious community venues [n = 9: i.e. senior centres [n = 4: nIRC = 1 [36], nEE = 3 [32, 35, 37]], bars [nEE = 1 [31]], community centres [n = 4: nIRHSC = 2 [32, 34], nEE = 2 [41, 42]], and a primary school [nEE = 1 [33]] or cultural or religious spaces [nEE = 2 [39, 40]]. One study (engaging African American and Latino adults with depressive symptoms) operated across both religious (faith centres) and non-religious spaces (senior centres and barber shops) venues [nEE = 1 [38]]. See Table 2 for further intervention delivery detail.
Targeted populations included: ‘gay and bisexual men’ [nEE = 1 [31]]; individuals ≥ 55 [n = 3: nIRC = 1 [36], nIRHSC = 1 [32], nEE = 1 [37]]; school students [nEE = 1 [33]]; ‘Black and minority ethnic groups’ [n = 5: nIRC = 1 [36], nEE = 4 [37,38,39,40]]; and, adults i) with type 2 Diabetes [nEE = 1 [41]], ii) with depressive symptoms (African Americans and Latinos) [nEE = 1 [38]], iii) up to two years post stroke [nIRHSC = 1 [34]] iv) who are obese [nEE = 1 [35]] and v) residing in North England (County Durham) [nEE = 1 [42]]. County Durham, a mixed rural and urban area, was of interest as resident health is typically poorer than the national average; the service aimed to predominately work with the county’s 30% most deprived communities (no further detail provided on how these communities were defined or identified) [42].
What designs, methods and outcomes measures have been used to produce cost and economic evidence?
Table 5 summaries the designs, methods and outcome measures used to produce the economic evidence on ABAs.
The study designs used to evaluate the ABAs included: cohort studies [n = 3: nIRHSC = 1 [32], nEE = 2 [31, 33])]; individual-level randomised controlled trials (RCTs) [n = 3: nIRC = 1 [36], nIRHSC = 1 [34] (feasibility trail for larger scale study), nEE = 1 [37]]; cluster RCTs (with ‘clusters’ typically corresponding to the community asset) [nEE = 4 [35, 38, 39, 41]]; a before and after study [nEE = 1 [42]]; and, a panel study [nEE = 1 [40]].
All studies compared, at the minimum, health/wellbeing outcomes against/between:
-
post intervention outcomes between participation/ non-participation [nIRHSC = 1 [32]];
-
pre- and post- intervention outcomes [nEE = 1 [33]];
-
four-month wait-list control group (the control group received the intervention four-months after the intervention arm) [n = 2: nIRC = 1 [36], nEE = 1 [37]];
-
non-ABA intervention (technical assistance offered through webinar and primary care site visits, ‘traditional’ style intervention delivered for the evaluation) [nEE = 1 [38]];
-
healthcare professional delivered service versus ABA lay worker delivered service [nEE = 1: [35]]
-
forecasted intervention outcomes through behaviour change models [nEE = 2 [31, 42]].
Primary outcome and secondary outcomes (either health/ wellbeing and/or economic outcomes) were explicitly specified in four papers: in one instance both were cost outcomes [nIRHSC = 1 [32]]; in two instances both were health outcomes [n = 2: nIRC = 1 [36], nIRHSC = 1 [34]]; and in a single instance both were measures of cost-effectiveness [‘Incremental cost effectiveness ratio’ (ICER): a summary measure, dividing the difference in total cost by the difference in the chosen measure of health outcome or effect; nEE = 1 [37]]. In all other cases health outcome was reported alongside aggregated cost or within cost-effectiveness measures (not identified as primary or secondary outcomes).
Health outcome measures utilised included: i) PHQ-9 and change in categorical diagnosis [nIRC = 1, [36]]; ii) infections averted and QALY gained [nEE = 1, [31]]; iii) ICECAP-A,Footnote 1 WEMWBS,Footnote 2 HADSFootnote 3; RSES,Footnote 4 SF-36 V.1Footnote 5 and HSDS-111Footnote 6 [nIRHSC = 1, [34]]; iv) achieved behaviour change [nEE = 1 [42]]; v) weight loss [nEE = 1 [39]]; and, vi) EQ-5D and HUI-3- derived QALY [nEE = 1, [37]].
Seven studies report aggregate cost [n = 7: nIRC = 1 [36], nIRHSC = 2 [32, 34], nEE = 4 [31, 33, 38, 41]], with five reporting cost within cost-effectiveness measures: ICER [nEE = 2 [37, 40]], ‘value for money’ assessment [nEE = 1 [42]] and ‘cost per kg loss’ [nEE = 2 [35, 39]].
What is the accrued evidence for the cost and economic impact of ABAs?
Table 6 summaries the accrued evidence for the cost impact of the ABAs. Gitlin 2012 [36] [clustered randomised trial], assigned to IRC, reported cost without comparison. Thus, a conclusion based on this paper, as to whether the ABA is cost-effective cannot be reached. The later published economic evaluation by Pizzi et al. [37] explores the cost-effectiveness of the ABA costed in the Gitlin 2012 [36] (details given below).
Category IRHSC consists of two studies. Similarly to Gitlin 2012 [36], Ellis-Hill 2019 [34] [feasibility study] reported cost without a comparison, thus cost-effectiveness cannot be determined [34]. The study notes the lack of suitable comparators within existing literature, precluding easily overcoming the lack of study comparator. Further, the authors make recommendations for more appropriate use of wellbeing measures to support evaluation of intervention impact. Within a retrospective cohort design, Mayer et al. [32] compared participating older adults within senior centres, against non-participating community members. Compared to the non-participants, during the year following the ABA, participants had lower, but non-significant (P = 0.58), total health care costs and no difference in hospitalisation. The authors note that ABA participants had significantly higher levels of comorbidity (P < 0.001) than the non-participant control. Thus, the comparison may be confounded by the typical increase in hospitalisation seen when comorbidity severity is higher: the ABA impact may be undervalued due to disparity in the study arms. Further, to assess bias, they assessed inclination to use preventative health services – the intervention arm had significantly higher scores, suggesting a stronger tendency to access/use services. Given this, Mayer 2010 [32] is suggestive of a dominant intervention [“A dominant treatment option is one that is both less costly and results in better health outcome than the comparator treatment” [43]].
Nine studies were categorised as EEs, with varying degrees of detail. Using a population-level model Kahn 2001 [31] estimated 5.0 to 6.2 HIV infections averted over five years, at a societal cost of $18,000 or less per infection averted (excluding savings from HIV medical costs averted). These authors emphasise different time frames, epidemic scenarios, cost perspectives and modelling inputs lead to a range in cost per infection averted ($4,500 to $46,400) [31]. They believe this compares favourably with other programmes (e.g. Biloxi: $12,000 to $65,000 per HIV case averted) [31]. When savings from HIV medical costs averted are included, the program “eliminates more in HIV medical costs than it costs to implement” (P. 487, [31]).
Stevens [40] used Monte Carlo simulation, estimating intervention costs of £56,986, and reduction in in smoking of 3–7%, resulting in a mean cost of just over £105 per life year gained [40]. Intervention success was noted, in particular, among those not in full time employment. No explicit statement about cost effectiveness was made by the authors. Krukowski [35] compared intervention implementation costs (training; recruitment; materials; ongoing implementation support) of $165 per participant to mean weight loss of 3.7 kg per participant, considered cost-effective compared to a professionally delivered service [35].
Pizzi [37] reported mean incremental costs of $146 per participant per month, with an incremental utility of 0.046 (EQ-5D derived). Base case ICERs, compared to 4-month control, were $64,896 per QALY (EQ-5D) and $36,875 per QALY (HUI-3). Sensitivity analysis yielded cost/QALY range of $20,500-$76,500. The study concludes cost effectiveness compared to threshold values [such thresholds are “the maximum amount a decision-maker is willing to pay for a unit of health outcome” [44]]. Pizzi et al. consider thresholds identified in the literature (US $50,000-$100,000/QALY), and previously reported range of ICERs for pharmacological and neurological depression interventions [37]. Eckermann [33] used an investment multiplier to assess cost effectiveness of an initial government grant, estimating the multiplier impact on total community activity (up to two years) was 5.07 ($226,737 against $44,758 invested). They label this as a successful return on investment (without comparison to any particular threshold), alongside success in health promotion and community network is concluded [33].
Wingate [41] conducted a cost comparison, arguing against a cost effectiveness analysis given no statistically significant difference in condition-specific outcome measure or quality of life assessment between alternatives. Per participant per annum, implementation costs were £13.84, out-of-pocket costs £11.41, but the NHS incurred a cost-saving £138.38 – overall, a saving of £113.13 [41]. Consequently, the authors conclude the intervention is cost effective, highlighting reductions in self-reported healthcare utilisation. Chung et al. [38] use a cost consequence framework, reporting disaggregated direct and indirect costs across various service sectors. The study comparator had lower overall costs, due to higher start-up costs (to engage and train staff and organisations within the ABA) and no significant differences in 12-month service use cost. However, the authors note capacity was successfully built within community staff, with information shared within the organisation, with potential longer-term benefits not captured in the 12-month evaluation. This omission was common across all studies – none valued the benefit of building capacity/upskilling staff.
Visram [42] conducted a value for money assessment. They estimated total public sector cost savings of £2,406,920 (health gain and cost saving to NHS: £1,477,911; costs offset to NHS from asset mapping and signposting: £798,800; social care: £126,326; criminal justice: £3,883) [42] against service delivery costs of £3,528,894, giving an overall cost of £1,121,974. With an unweighted total health gain of 287.7 QALYs, this results in a cost per QALY of £3,900. Thus, the intervention was deemed cost effective against National Institute for Health and Care Excellence recommended threshold value £20,000-£30,000 per QALY gained [42].
Yeary [39] report per participant mean intervention costs of $348.95 and mean weight loss of 2.53 kg, resulting in a cost of $138 per kg lost. They argue their results indicate cost effectiveness but refrain from giving a concluding statement, due to concerns around the appropriateness of the comparator [there was no ‘true’ control group as both arms received the same core weight loss programme, with the intervention arm receiving a further 12 maintenance sessions]. Mean weight loss was higher in the ABA intervention than a real world setting comparison, based on literature values (an intervention causing an additional 2.1 kg weight loss compared to control) [39]. The authors report challenges to overcoming the lack of intervention comparator through utilising literature values, emphasising that in previous literature costs and outcomes were not reported separately by race: “Given blacks typically loose less weight than white in behavioural weight loss interventions, cost per pound lost may be considerably higher among blacks” (P.2, [39]).
Overall, three papers, representing two ABAs explicitly, report that interventions were well received/ enjoyed/ appreciated by participants, noting them as highly valued or increasing confidence both during intervention participation and beyond (n = 3: nIRC = 1 [36], nIRHSC = 1 [34], nEE = 1 [37]). No paper reported this using formal research methods – either qualitatively or through metrics – rather relying on informal research observations. The same studies explicitly mention good engagement and ‘buy-in’ from ABA facilitators.
Discussion
What designs, methods and outcomes measures have been used to produce cost and economic evidence?
ABAs in principle seem desirable given pressure to reduce demand on public services and find ways to mitigate inequalities. However, the economic literature about them is extremely limited. A high proportion of included studies suggest that ABAs are cost-effective, a result potentially subject to publication bias, whereby only evidence from ABAs with positive economic findings are published, skewing the published evidence base. If present, as time progresses, publication bias becomes increasingly concerning as “in the presence of publication bias, belief in the relationship increases iteratively with each positive publication” (P.150, [45]). However, with this important caution in mind, we observed: all included ABAs claimed to successfully target and engage underserved, minority or vulnerable populations; such claims would be better substantiated with more formalised capture of participant socioeconomic status. Among the included papers, methods varied, not only in design and comparators, but also in terms of included costs, and outcome measures, likely reflecting the broad scope of ABAs. The prescriptive nature of economic evaluation frameworks may constrain ABA evaluation. Short comings were noted, in both undervaluing of health and wellbeing outcomes, the impact on those beyond the main intervention recipients and short term (time horizon) follow-up of the evaluation.
While studies claimed engagement of underserved populations, none formally reported measured socioeconomic status of participants. Whilst target populations may be assumed, or considered, marginalised, underserved, or residents of more deprived localities, inequality could be better assessed through measurement of socioeconomic status (e.g. income level) or deprivation [e.g. in the UK postcodes (a series alphanumeric characters denoting geographical area used within postal addresses) can be used as a proxy measure for socioeconomic status using established datasets e.g. Index of Multiple Deprivation]. For example, it cannot be known if the more affluent community members (or people who travelling from other more affluent communities) were attending these groups, potentially subverting the ABA aim of engaging the most deprived or marginalised. The importance of this concern will vary by community: if every community member is considered ‘deprived’, engaging any member may be of value. Given the equity improvement focus, more information about the communities in which the ABAs are delivered may help further inform implementation. Reporting of these factors is needed to meaningfully value and prioritise ABAs as a whole and assess their position in inequality improvement – particularly in the context of scare public sector resources. In isolation, ABAs may not fully solve problems of engagement of the underserved but may go some way to resolving them.
Careful consideration should be given to the contextual appropriateness of ABAs. ABAs are useful as they utilise existing resources and can effectively engage people not normally reached. However, it presumes that localities have resources upon which to build. Thus, inequalities may be perpetuated were ABAs to be utilised exclusively: communities short of assets may continue to receive no additional interventions. Thus, exclusively relying on ABAs may perpetuate some inequalities. Perhaps, optimally, one might consider ABAs as one ‘tool’ within a wider ‘toolkit’ of approaches for engaging underserved individuals.
Health outcomes were measured within all publications. Ellis-Hill 2019 [34] explored outcome measures for a larger trial and was the only study to include holistic capability measures (e.g. WEMWBS or ICECAP-A). The authors concluded that measures of emotional well-being would be the most relevant study outcome. This adds evidence to the argument that health specific measures (e.g. QALYs) may not fully capture benefits in this setting – ABAs may be better evaluated using more generic measures of wellbeing. Three studies also explicitly reported improvements in participant ‘enjoyment’, yet this was not measured, in any capacity, within the utilised costing frameworks. Consequences of social gain (e.g. increasing social confidence to support future engagement or gaining knowledge of services through naturalistic conversations) and emotional well-being improvements should also be considered – holistic capability measures may capture some of these effects.
In ABA evaluation, costs and time horizon need to be carefully considered. Where set-up and training costs are included in intervention delivery costings, ABAs may be disadvantaged if they are compared over short time horizons (1–2 years) – it may be better to consider them one-off set-up costs. However, costing should consider costs of training new staff, maintaining staff, and other ongoing costs – sensitivity analyses may be useful for exploring such points. Further, short time horizons made evidencing long-term impact, and subsequent costs, challenging.
A general challenge of evaluations of preventative or complex interventions, also evidenced here, is capturing the wider life course benefit accrued from engagement with behaviour change interventions. Without a complete retrospective dataset, with a large sample size and an appropriate comparator, it is challenging to definitively assess the impact of such interventions. It is also unknown what would have happened in the absence of the intervention. In some instances (e.g. [31] and [42]), authors made attempts to overcome this by utilising established behaviour change models in their evaluations, including sensitivity analysis to understand the impact of adopted assumptions. However, these models may undervalue ABA contributions if benefits are valued on their contribution/ outcome in the general population (c.f. the earlier consideration of differing weight loss value in white versus black populations).
A key ABA feature, building community capacity, was not captured in costing evaluation frameworks. Given employment is recognised as a ‘social determinant of health’ and a key influencer on overall personal wellbeing, upskilling staff and the wider community, it may well have consequences beyond the intervention focus [46, 47]. Building capacity among staff may offer improved employment opportunities—increasing income—positively contributing to staff’s social determinates of health, potentially reducing their use of health and wellbeing services. However, unmentioned in any included study, is how this may contribute to staff-turnover, perhaps increasing recruitment and training costs.
Relatedly, ABAs are also undervalued where ‘spill over’ effects are not considered, which is of concern since ABAs often impact beyond intervention recipients (e.g. information is shared beyond the sample population to others in the target population or capacity is built among asset staff). Economic evaluation frameworks typically capture the intervention impact on the group of participating individuals. Social return on investment [a “…performance measure similar to ‘return on investment’ but takes a broader societal perspective to valuing cost and benefits. Social and environmental factors are considered, in addition to economic variables to estimate benefit and cost” [48]] may be better suited to captured the wider social and environmental benefits of the intervention, including benefits of building capacity among staff.
Another overlooked cost includes failed engagement of assets – approaching a community asset for an ABA, possibly even developing a unique approach to match their space, population needs, staffing etc., and the proposed intervention not commencing. Publication bias likely plays a role here – if the intervention does not commence, then there is little to evaluate and report/publish. Such costs should be considered to ensure realistic and appropriate costing of ABA implementation.
What is the accrued evidence for the cost and economic impact of ABAs?
Among the identified studies assessing cost-effectiveness, in all but one [38] ABAs were found to be cost-effective, either delivering benefits at a lower cost than an alternative or accruing additional benefits at an acceptable additional cost. However, authors acknowledge the robustness of these conclusions was diminished by the appropriateness of utilised comparators. Inherent to ABA interventions are engaging specific populations, linked to an existing asset in a specific localised area. Consequently, randomisation options are significantly impacted: individual level randomisation will often be infeasible. Therefore, outcome comparisons may be confounded by factors such as population differences. This may be alleviated in part by using analysis that adjusts for such differences: for example, when comparing outcomes between those engaging and not engaging in the intervention, it may be wise to adjust for inclination to engage with services, as discussed in Mayer 2010 [32]. However, this can only address known and measured confounders. Some studies utilised a comparison between participant and non-participants (e.g. [32]): however, the validity of this design may be decreased with some ABA interventions, where ‘participation’ may not always be clear-cut (for example in information sharing interventions) – statistical contamination may occur between comparison groups.
Some evaluations had no comparator. Among these, some sought to compare outcomes to values from literature to demonstrate beneficial impacts. However, two studies noted they were inhibited from doing so because of a lack of relevant literature. This reinforces the more general consideration of the need for improved representation of underserved populations in literature. This general goal may be supported through disaggregating study data by population group (e.g. sub-group analysis).
Some ABAs promote access to other health and wellbeing improvement services, employment, and job services. From the current evidence base it is unclear whether ABA participation does indeed support access to secondary services. A key motivation for utilising ABAs is to help people from disengaged populations to take preventative action, potentially reducing their future use of other health and social care resources. By failing to measure the impact on wider health and wellbeing services, the value of ABAs may be either i) grossly undervalued or ii) missing costly impacts on wider services. Such considerations are also impacted by the adopted time horizon: health and social service costs may rise in the short term (e.g. increased use of screening services).
As the emphasis on community intervention grows, ABAs, and their economic evidence, should be contextualised to the current economic and political climate. For example, the publication gap 2020–23 may be a consequence of the COVID-19 pandemic. Community assets suffered because of government-imposed restrictions preventing in-person gatherings, diminishing community participation. As we move toward to a post lockdown era, entering a cost-of-living crisis, there is significantly higher demand on community assets (such as libraries or foodbanks). Consequently, adopting an ABA and ‘asking’ more of community assets should be considered with caution. For example, in a number of the ABAs evaluated, there was no mention of venue or room hire costs; with current rising costs, the ability of assets to ‘absorb’ increased costs (e.g. hiring a room for longer to deliver a ABA) is likely significantly reduced. Consequently, policy makers should consider if it is sustainable, or indeed ethical, to ‘push’ the responsibility of ABAs on to already stretched assets.
In conducting this review, we found many of the excluded screened papers made mention of ABAs being ‘economically efficient’ without formally evaluating this domain. It is important such claims are validated with evidence, so that the reality of implementation is known. Further, publications generally lacked details on implementation strategies, resulting in the possible exclusion of some papers which may have been an ABA. As the weight of evidence of community intervention increases, implementation strategies should be routinely reported, and consistent terminology employed. This allows for an inference of community impact, in the instances where economic impact fails to fully capture the contextualised social value.
Conclusions
Economic literature on ABAs is extremely limited. ABAs seem to be a promising way to successfully target and engage underserved, minority or vulnerable populations, and may not result in a higher net cost when compared to other approaches to health and wellbeing improvement. The included ABAs represent a broad range of approaches, with methods of evaluation varying widely, not only in design and comparators, but also in terms of included costs, and outcome measures. The current use of economic evaluation methodologies do not capture well the full impacts of ABAs, likely both undervaluing health and wellbeing outcomes (i.e. capacity building, holistic health improvements, increased secondary health and wellbeing service use, and long-term impact on health) and staff capacity building, as well as underestimating delivery costs (i.e. venue higher and failed asset engagement). Current economic evidence struggles due to lack of appropriate intervention comparator, made challenging by the hyper-local nature of ABAs.
In health economics generally, interventions are typically considered as mutually exclusive occurrences, however in the context of community health, and specifically ABAs, this approach typically misses the economic reality of embedding services. The economics of the surrounding services, mechanisms of information sharing, and collaboration underpin the success of assets and ABAs. The economic evidence, and evaluations in general, would benefit from further detail to help ensure more nuanced and sophisticated application of ABAs. Further evidence is needed to determine the cost-effectiveness of ABAs.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Notes
ICEpop CAPability measure for adults.
Warwick-Edinburgh Mental Well-being Scale.
Hospital Anxiety and Depression Scale.
Rosenberg Self-Esteem Scale.
Medical Outcomes Short Form Health Survey.
Head Injury Semantic Differential Scale.
Abbreviations
- ABAs:
-
Asset-based approaches
- CASP:
-
Critical Appraisal Skills Programme
- CENTRAL:
-
Cochrane Centre Register of Controlled Trials
- CHW:
-
Community Health Workers
- EE:
-
Economic evaluation
- EoE:
-
East of England
- EQ-5D:
-
EuroQol five dimension questionnaire
- HADS:
-
Hospital Anxiety and Depression Scale
- HDS-111:
-
Head Injury Semantic Differential Scale
- ICE-CAP-A:
-
ICEpop CAPability measure for adults
- NHS:
-
National Health Service
- PHQ-9:
-
Patient Health Questionnaire – 9
- PPI:
-
Patient and public involvement
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QALY:
-
Quality adjusted life-years
- RSES:
-
Rosenberg Self-Esteem Scale
- SF-36 V.1:
-
Medical Outcomes Short Form Health Survey
- WALYs:
-
Wellbeing adjusted life years
- WELBYs:
-
Wellbeing adjusted life years
- WEMWBS:
-
Warwick-Edinburgh Mental Well-being Scale
References
Alderwick H, Dunn P, Mckenna H, Walsh N, Ham C. Sustainability and transformational plan in the NHS: How are they being developed in practice? [report]. The King's Fund; 2016. Available from: https://www.kingsfund.org.uk/insight-and-analysis/reports/stps-in-the-nhs.
Van Tine B, Nuwan Darshana W, Antony M, Steven M. Health assets in a global context: a systematic review of the literature. BMJ Open. 2019;9(2):e023810.
Brooks F, Kendall S. Making sense of assets: what can an assets based approach offer public health? Crit Public Health. 2013;23(2):127–30.
Morgan A, Ziglio E. Revitalising the evidence base for public health: an assets model. Promot Educ. 2007;Suppl 2:17–22.
Baker D. Developing and implementing a robust asset-based approach to public health. Perspect Public Health. 2014;134(3):129–30.
NHS. About the NHS Long Term Plan. 2019. Available from: https://www.longtermplan.nhs.uk/about/.
Scottish community development centre. Asset Based Approaches. 2019. Available from: https://www.scdc.org.uk/what/assets-scotland.
Scottish Public Health Observatory. Assets Public Health Infromation for Scotland. 2019. Available from: https://www.scotpho.org.uk/life-circumstances/assets. Updated 24 October 29.
Morgan A, Ziglio E. Revitalising the evidence base for public health: an assets model. Promot Educ. 2007;14(2_suppl):17–22.
Community Development Practice Hub. ABCD Institue Chicago USA. 2021. Available from: https://www.bvsc.org/abcd-institute-chicago-usa.
Glasgow Centre for Population Health. Putting asset based approaches into practice: identification, mobilisation and measurement of assests [report]. Glasgow; 2012. Available from: https://www.gcph.co.uk/publications/362_concepts_series_10-putting_asset_based_approaches_into_practice.
Hanson S, Jones A. A spatial equity analysis of a publuc health intervention: a case study of an outdoor walking group provider within local authorities in England. Int J Equity Health. 2015;14:106.
Acheson D. Independent Inquiry into Inequalities in Health Report. 1998.
Rippon S, Hopkin T. Head, hands and heart: asset-based approaches in health care [report]. London: The Health Foundation; 2015. Available from: https://www.health.org.uk/publications/head-hands-and-heart-assetbased-approaches-in-health-care.
Rippon S, South J. Promoting Asset Based Approaches for Health and Wellbeing: Exploring a Theory of Change and Challenges in Evaluation [report]. Leeds: Leeds Beckett; 2017. Available from: https://eprints.leedsbeckett.ac.uk/id/eprint/4497/.
Herlitz L, Macintyre H, Osborn T, Bonell C. The sustainability of public health interventions in schools: a systematic review. Implement Sci. 2020;15(1):4.
Zaza S, Briss P, Harris K. Understanding and using economic evidence. Task Force on Community Service: the Guide to Community Prevention Services, What Works to Promote Health? New York: Oxford University Press; 2005. p. 449–63.
Payne K, McAllister M, Davies LM. Valuing the economic benefits of complex interventions: when Maximising health is not sufficient. Health Econ. 2013;22(3):258–71.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021;74:n2061.
Johnson R, Jenkinson D, Stinton C, Taylor-Phillips S, Madan J, Stewart-Brown S, et al. Where’s WALY? : A proof of concept study of the ‘wellbeing adjusted life year’ using secondary analysis of cross-sectional survey data. Health Qual Life Outcomes. 2016;14(1):126.
Brazier J, Ratcliffe J, Saloman J, Tsuchiya A. Measuring and Valuing Health Benefits for Economic Evaluation. 2nd ed. Oxford University Pres; 2016.
Wildman J, McMeekin P, Grieve E, Briggs A. Economic evaluation of integrated new technologies for health and social care: Suggestions for policy makers, users and evaluators. Soc Sci Med. 2016;169:141–8.
Byford S, Raftery J. Perspectives in economic evaluation. BMJ. 1998;316(7143):1529–30.
Baltussen R, Marsh K, Thokala P, Diaby V, Castro H, Cleemput I, et al. Multicriteria Decision Analysis to Support Health Technology Assessment Agencies: Benefits, Limitations, and the Way Forward. Value in Health. 2019;22(11):1283–8.
Cookson R, Drummond M, Weatherly H. Explicit incorporation of equity considerations into economic evaluation of public health interventions. Health Econ Policy Law. 2009;4(2):231–45.
Edwards RT, Charles JM, Lloyd-Williams H. Public health economics: a systematic review of guidance for the economic evaluation of public health interventions and discussion of key methodological issues. BMC Public Health. 2013;13(1):1001.
Lindholm LA, Emmelin MA, Rosén ME. Health maximization rejected: the view of Swedish politicians. Eur J Public Health. 1997;7(4):405–10.
Kocot E, Kotarba P, Dubas-Jakóbczyk K. The application of the QALY measure in the assessment of the effects of health interventions on an older population: a systematic scoping review. Arch Public Health. 2021;79(1):201.
Moher D LA, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine. 2009;6:e1000097.
Critical Appraisal Skills Programme. CASP Checklist; 2019. Available from: https://casp-uk.net/referencing/.
Kahn JG, Kegeles SM, Hays R, Beltzer N. Cost-effectiveness of the Mpowerment Project, a community-level intervention for young gay men. J Acquir Immune Defic Syndr. 2001;27(5):482–91.
Mayer C, Williams B, Wagner EH, LoGerfo JP, Cheadle A, Phelan EA. Health care costs and participation in a community-based health promotion program for older adults. Prev Chronic Dis. 2010;7(2):A38.
Eckermann S, Dawber J, Yeatman H, Quinsey K, Morris D. Evaluating return on investment in a school based health promotion and prevention program: the investment multiplier for the Stephanie Alexander Kitchen Garden National Program. Soc Sci Med. 2014;114:103–12.
Ellis-Hill C, Thomas S, Gracey F, Lamont-Robinson C, Cant R, Marques EMR, et al. HeART of Stroke: randomised controlled, parallel-arm, feasibility study of a community-based arts and health intervention plus usual care compared with usual care to increase psychological well-being in people following a stroke. BMJ Open. 2019;9(3):e021098.
Krukowski RA, Pope RA, Love S, Lensing S, Felix HC, Prewitt TE, et al. Examination of costs for a lay health educator-delivered translation of the Diabetes Prevention Program in senior centers. Prev Med. 2013;57(4):400–2.
Gitlin LN, Harris LF, McCoy M, Chernett NL, Jutkowitz E, Pizzi LT. A community-integrated home based depression intervention for older African Americans: [corrected] description of the Beat the Blues randomized trial and intervention costs. BMC Geriatr. 2012;12:4.
Pizzi LT, Jutkowitz E, Frick KD, Suh DC, Prioli KM, Gitlin LN. Cost-effectiveness of a community-integrated home-based depression intervention in older African Americans. J Am Geriatr Soc. 2014;62(12):2288–95.
Chung B, Ong M, Ettner SL, Jones F, Gilmore J, McCreary M, et al. 12-Month cost outcomes of community engagement versus technical assistance for depression quality improvement: a partnered, cluster randomized, comparative-effectiveness trial. Ethn Dis. 2018;28(Suppl 2):349–56.
Yeary KHK, Kaplan CM, Hutchins E. Implementation costs of a community health worker delivered weight loss intervention in black churches serving underserved communities. Prev Med Rep. 2020;18:101084-.
Stevens W, Thorogood M, Kayikki S. Cost-effectiveness of a community anti-smoking campaign targeted at a high risk group in London. Health Promot Int. 2002;17(1):43–50.
Wingate L, Graffy J, Holman D, Simmons D. Can peer support be cost saving? An economic evaluation of RAPSID: a randomized controlled trial of peer support in diabetes compared to usual care alone in East of England communities. BMJ Open Diabetes Res Care. 2017;5(1):e000328.
Visram S, Walton N, Akhter N, Lewis S, Lister G. Assessing the value for money of an integrated health and wellbeing service in the UK. Soc Sci Med. 2020;245:112661.
York Health Economics Consortium. Dominance; 2016. Available from: https://yhec.co.uk/glossary/dominance/.
York Health Economics Consortium. Cost-Effectiveness Threshold York. 2016. Available from: https://yhec.co.uk/glossary/cost-effectiveness-threshold/.
Joober R, Schmitz N, Annable L, Boksa P. Publication bias: what are the challenges and can they be overcome? J Psychiatry Neurosci. 2012;37(3):149–52.
Armenti K, Sweeney MH, Lingwall C, Yang L. Work: a social determinant of health worth capturing. Int J Environ Res Public Health. 2023;20(2):1199.
Office for National Statistics. What matters most to personal well-being? 2013. Available from: https://webarchive.nationalarchives.gov.uk/ukgwa/20160107113217/http:/www.ons.gov.uk/ons/rel/wellbeing/measuring-national-well-being/what-matters-most-to-personal-well-being-in-the-uk-/sty-personal-well-being.html.
York Health Economics Consortium. Social Return on Investment. 2016. Available from: https://yhec.co.uk/glossary/social-return-on-investment/.
Acknowledgements
Dr. Rory Cameron. University of East Anglia
Dr. Jurgen Grotz, University of East Anglia
Dr. Guy Peryer. University of East Anglia
Helen Risebro, University of East Anglia
Nadia Jones, Local Authority Stakeholder
Funding
This study is funded by the National Institute for Health and Care Research (NIHR) Applied Research Collaboration East of England (NIHR ARC EoE) at Cambridgeshire and Peterborough NHS Foundation Trust. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
LB's time was supported by the NIHR Applied Research Collaboration East of England Inclusive Involvement in Practice-led Research theme.
Author information
Authors and Affiliations
Contributions
AW acted as the main contributor on this review, contributing to and leading on each stage. LB contributed to the conception and design of the review, as well as the identification of papers, analysis, and revisions to the manuscript. JW and SH contributed to the design, methods and revisions on the manuscript. JW also supported paper identification by resolving conflicts. SC, acted as PPI, contributing to the conception, design, data extraction and interpretation of data. APW closely supervised AW on each stage of this project, acting as a major contributor to the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wreford, A., Birt, L., Whitty, J.A. et al. Cost and economic evidence for asset-based approaches to health improvement and their evaluation methods: a systematic review. BMC Public Health 24, 814 (2024). https://doi.org/10.1186/s12889-024-18231-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18231-4