- Research
- Open access
- Published:
Assessment of global antimicrobial resistance campaigns conducted to improve public awareness and antimicrobial use behaviours: a rapid systematic review
BMC Public Health volume 24, Article number: 396 (2024)
Abstract
Introduction
Public health campaigns with a well-defined outcome behaviour have been shown to successfully alter behaviour. However, the complex nature of antimicrobial resistance (AMR) creates challenges when evaluating campaigns aimed at raising awareness and changing behaviour.
Aims
To determine what campaigns have been conducted and which reported being effective at improving awareness of antimicrobial resistance and changing behaviour around antimicrobial use in members of the public. It also sought to determine the outcome measures studies have used to assess campaign effectiveness.
Methods
A systematic search of Ovid MEDLINE and Embase, was conducted in October 2022 using a predefined search strategy. Studies which were published between 2010 and September 2022 that outlined a campaign or invention aimed at the public and focusing on AMR or antibiotic usage were eligible for inclusion and studies which solely targeted healthcare professionals (HCP) were excluded.
Results
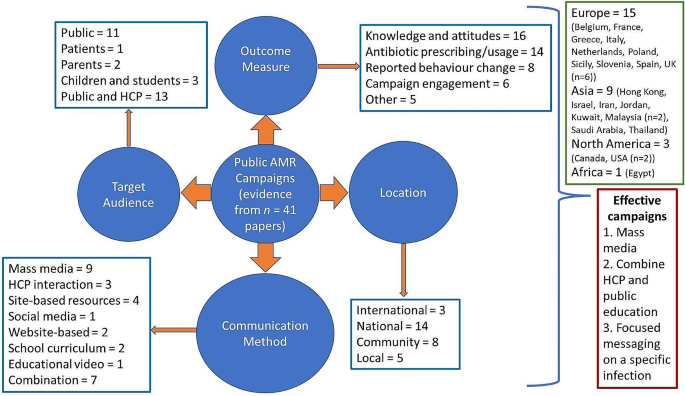
Literature searches retrieved 6961 results. De-duplication and screening removed 6925 articles, five articles from grey literature and reference screening were included, giving a total of 41 studies and 30 unique interventions. There was a distribution of campaigns globally with the majority run in Europe (n = 15) with most campaigns were conducted nationally (n = 14). Campaigns tended to focus on adult members of the public (n = 14) or targeted resources towards both the public and HCPs (n = 13) and predominately assessed changes in knowledge of and/or attitudes towards AMR (n = 16). Campaigns where an improvement was seen in their primary outcome measure tended to use mass media to disseminate information, targeted messaging towards a specific infection, and including the use of HCP-patient interactions.
Discussion
This review provides some evidence that campaigns can significantly improve outcome measures relating to AMR and antibiotic usage. Despite a lack of homogeneity between studies some common themes emerged between campaigns reported as being effective. However, the frequent use of observational study designs makes it difficult to establish causation between the campaign and changes seen in the studies outcome measures. It is important that clear evaluation processes are embedded as part of the design process for future campaigns; a campaign evaluation framework for use by campaign developers may facilitate this.
Introduction
Antimicrobial resistance (AMR) has become a major public and global health challenge with an estimated 4.95 million deaths associated with bacterial AMR in 2019 [1]. Following the publication of a Global Action Plan in 2015 and subsequent UN declaration signed by 193 countries, several countries have published and are implementing national policies to tackle AMR [2, 3].
Inappropriate prescribing, especially for viral infections, such as respiratory tract infections (RTIs) [4], is one of the main driving factors for increasing levels of AMR. Most antibiotics are prescribed in primary care [5], a setting with significant interaction between the healthcare professional (HCP) and patient. Patient expectation and perceived patient expectation are often cited by general practitioners (GPs) as the main reasons for prescribing an antibiotic to treat a RTI [6, 7]. A meta-analysis showed that physician’s perception of patient desire for antibiotics and patient desire for antibiotics were associated with antibiotic prescribing for RTIs (odds ratio (OR): 2·11 to 23·3 and 0·61 to 9·87 respectively) [6]. In addition to the potential influence patients have during HCP-patient interactions in primary care, public behaviours such as self-medication [8] and inappropriate disposal of antibiotics [9] can also impact on AMR. Therefore, the lack of public knowledge regarding AMR and appropriate antibiotic usage, which has been identified through public surveys, is concerning [10].
Public health campaigns have been successful in improving knowledge and changing behaviour in other areas of public health [11, 12]. However, developing a public health campaign focused on AMR is challenging due to the complexity of both campaign messaging and the behaviour contributing towards increasing AMR. This also presents challenges when evaluating the campaign as there are certain scenarios where antibiotic prescribing is necessary and appropriate and some outcome measures may not reflect individual behaviours. Furthermore, previous reviews have restricted campaigns included by study design of the evaluating study [13], type of outcome measure used [14], or type of intervention implemented [3], and therefore do not provide an overall summary of campaigns and interventions which have been conducted to alter behaviour around antibiotic usage.
Therefore, this review aimed to determine what public campaigns to improve public awareness and antimicrobial use behaviours have been conducted worldwide and which of these have been effective at improving awareness of AMR or changing behaviour around antimicrobial use in members of the public. It also sought to determine what outcome measures were used to assess whether the campaign effectively altered factors known to contribute towards AMR.
Methods
The review follows the PRISMA 2020 item checklist (Supplementary Material 1.) and is registered with PROSPERO (registration number CRD42022371142). The rapid review methodology was chosen due to the need to disseminate findings quickly to inform the development of the future AMR National Action Plan, however, this methodology does come with some limitations [15]. Abbreviated methods were followed with papers screened by one reviewer and 4% of full text screened papers reviewed by a second reviewer. Data extraction was also conducted by one reviewer. Given the heterogeneity of study designs and outcome measures, data was synthesised using a narrative synthesis.
Search strategy
A PICO framework [16] was used to develop the main search terms, search strategies are shown in Supplementary Material 2. The database searches were performed on 5 October 2022 using Ovid Medline ALL and Ovid Embase with date limits 1 January 2010 to 4 October 2022. Conference abstracts were removed from the Embase search before download.
All records were imported into an Endnote library; after deduplication there were 4755 unique records. All 4755 citations were then imported into Rayyan, and 50 further duplicates were removed. Additionally, a grey literature search of Google identified 73 further unique citations and the reference lists of four systematic reviews identified from the search [3, 13, 14, 17] were screened to identify nine additional papers for screening. These citations were screened on title and abstract, and 557 (475 from published literature, 82 from grey literature and citation searching) were included for full text analysis. A PRISMA diagram (Supplementary Material 3.) depicts the flow of information through the review.
Screening
Due to the large number of articles retrieved by the search, articles were initially screened by searching for the terms campaign and/or intervention in Rayyan with articles included for further consideration if they included these terms. Following this, abstracts were reviewed by one reviewer to determine whether the paper met the inclusion criteria. If insufficient information was included in the abstract to determine whether the paper met the inclusion criteria the full paper was screened. For any papers where it was not clear if they fully met the inclusion criteria consensus was gained from a second reviewer.
Selection criteria
Studies which outlined a campaign or invention aimed at the public or patients and focusing on AMR or antimicrobial usage were considered. All study designs (except systematic reviews) and outcome measures were included, to allow data to be gathered on methods to assess measurable behaviour change resulting from an AMR campaign or intervention. Studies which solely targeted HCP were excluded to distinguish between interventions aimed at HCP and at the public. The inclusion and exclusion criteria applied can be found in Table 1.
Data extraction
A data extraction tool was designed with specified column headings using Microsoft Excel. Data was extracted in line with the main aims of the review to provide information on the study design, country within which the campaign was conducted, the study sample, intervention (main components, year of implementation, duration and key messages), the intervention target population (public, patient or combined), campaign or intervention type (international, national, community or local), the comparator used to determine effectiveness, outcome measures used (antibiotic prescribing or consumption, knowledge, attitudes and awareness of AMR, behaviour change and campaign recognition), and the study’s key findings.
Results
The literature search produced 6961 results. De-duplication removed 2206 results and the titles of the remaining 4705 results were screened resulting in the removal of a further 4230 studies. Following this, 475 results underwent further screening, with 36 studies meeting the inclusion criteria. An additional nine results were identified through systematic review bibliography screening, and 73 during grey literature searches, of which five results met the inclusion criteria, giving a total of 41 studies (30 unique interventions) to be included (Supplementary Material 3.).
Table 2. provides an overall summary of the studies included within this review and Table 3. Outlines the key focus of the included campaigns. The search showed a range of countries, both high and middle income, within which AMR campaigns or interventions had been conducted. However, most campaigns were conducted in high income countries (n = 23) [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40], with six campaigns conducted or originally developed within the UK [35, 39,40,41,42,43], and four [44,45,46,47] and two [48, 49] campaigns conducted in upper and lower middle-income countries respectively. A summary of the campaign characteristics is available in Fig. 1.
Study design
The majority of studies used cross-sectional [18, 21, 27, 29, 30, 34, 35, 37, 40, 42, 45, 47, 50,51,52,53] or longitudinal study designs [19, 20, 22, 24, 38, 39, 44, 46, 53, 54], (n = 14 and 10 respectively). five used a quasi-experimental [25, 32, 33, 36, 49] and two used an experimental design [23, 56].
Target population
The primary focus of 17 of the campaigns was the public [19, 21, 23, 24, 30, 33, 35, 38, 46, 49, 55], with two school curriculum-based campaigns focused on children [26, 27, 42, 47], two further campaigns focused on parental education [20, 44], and one campaign focused on patients [56]. The remaining 12 campaigns targeted both HCP and the public [18, 22, 25, 28, 29, 31, 32, 36, 45, 48, 57, 58].
Campaign type and communication methods predominantly used
Most were national campaigns (n = 13) which used mass media to disseminate information (n = 7) [19, 21, 22, 24, 38, 39, 45]. Other national campaigns used the school curriculum [47], social media [31], websites [29, 37], and interactions with HCP combined with education resources [28, 36] to communicate with their target audiences. Eight studies evaluated community or regional-level campaigns, with site-based resources, such as poster displays and leaflets, the most common communication method (n = 5) [20, 25, 32, 48, 49]. Local campaigns used HCP interaction (n = 2) [46, 56] and site-based resources, such as posters (n = 3) [30, 35, 40]. Finally, three international campaigns were identified which used mass media [58], school curriculums [26, 27, 42], and website content [37] to disseminate information.
Outcome measures
Change in participants knowledge of and/or attitudes towards AMR was predominantly used as an outcome measure (n = 16) [22, 23, 30, 33, 34, 38, 39, 43, 46,47,48,49,50,51, 55, 59]. Trends or changes in antibiotic prescribing or usage was also commonly used (n = 14) [18, 19, 21, 23–24, 32, 36, 48, 52,53,54,55, 60]. Other outcome measures used included reported behaviour change (n = 8) [23, 37,38,39, 49, 51, 56, 57], campaign engagement (n = 6) [29, 31, 50, 51, 57, 61], expenditure on antibiotics (n = 2) [19, 21], annual number of GP consultations (n = 1) [21], severity of respiratory tract infection symptoms (n = 1) [35], and perception of campaign messaging (n = 1) [62].
Changes in knowledge, attitudes, and behaviour
Table 4. summarises studies which assessed changes in knowledge, attitudes and behaviour following the campaign. Studies reviewing the pledge-based Antibiotic Guardian campaign assessed self-reported change in knowledge which shows 44·5% of Antibiotic Guardians reported an increase in knowledge post-campaign. This was more likely in individuals with limited pre-campaign knowledge of AMR (OR: 4·21, CI: 2·04–8·67) [37]. Furthermore, when making a pledge, Antibiotic Guardians were asked five knowledge-based questions. Comparison of these to Eurobarometer questionnaire responses by the UK or EU public showed Antibiotic Guardians answered more questions correctly (OR: 8·5 and 13·9 respectively) [51, 63]. However, not all studies analysing the Antibiotic Guardian campaign reported positive findings only. A qualitative analysis by Kesten et al. showed that a limited number of Antibiotic Guardians could fully recall their pledge and reports regarding improved knowledge following participation in the campaign were mixed [57].
Multiple campaigns used a pre- and post-campaign comparison of a knowledge-based questionnaire to determine the campaign’s effectiveness. Ho et al. showed a significant increase in knowledge regarding the ineffectiveness of antibiotics at treating viral infections following a mass media campaign promoting the key message “Antibiotics do not help in cold and flu” [22]. Thong et al. and Shehadeh et al. assessed the effect of one-to-one educational sessions conducted by HCPs; both showed significant improvements in knowledge of antibiotic use and resistance [44, 46]. Another intervention using a taught component delivered education sessions to school children as part of the school curriculum in Malaysia [47]. Assessment of knowledge showed a significant improvement in both mean knowledge and attitude scores as well as a correlation between the two scores. Finally, using independent samples, Mazinska et al. evaluated the impact of European Antibiotic Awareness Day (EAAD) in Poland [34]. Questionnaire data was collected from a random sample of adults aged over 18-years pre and post EAAD in 2009, 2010 and 2011 and showed those who were aware of the EAAD campaign (29·0% of respondents) had significantly better knowledge of appropriate antibiotic usage than those who were not aware of the campaign, especially regarding the use of antibiotics to treat RTIs [34].
A British public antibiotic campaign launched in 2008 was also evaluated using pre- and post-campaign questionnaire data [39]. While recognition of campaign materials, such as posters, increased over the campaign period, there was no significant change in attitudes, including attitudes towards the use of antibiotics to treat colds and flu despite this being the campaign’s key message. Furthermore, no significant change in self-reported antibiotic use occurred following the campaign. However, the latter Keep Antibiotics Working campaign showed significant improvements in some aspects of public knowledge [43]. Campaign recognition was higher than for the 2008 campaign (23·7 vs. 71·0%) and knowledge increased significantly for AMR specific questions such as “antibiotics will stop working if taken for the wrong things”. Levels of concern about AMR within the public also increased significantly post-campaign.
Changes in antibiotic prescribing
Table 5. summarises findings from studies which used antibiotic prescribing rates as their primary outcome measure. Studies that determined the effectiveness of the 2002 French mass media campaign used antibiotic prescribing data, obtained from several sources including prescribing panels, sales data from IMS Health France, government organisations, and National Insurance reimbursement data, as a primary outcome measure [21, 52,53,54]. These studies indicated a significant reduction in antibiotic prescribing with reductions of up to 33·0% during the final campaign period from 2009 to 2010. This effect however was not consistent across age groups with greater reductions seen in children compared to older adults, which is thought to be due to the introduction of the pneumococcal conjugate (7-valent) vaccine for children aged less than 5-years old [54]. Furthermore, Dunais et al. also analysed a local intervention which commenced in 2001 and ran alongside the national campaign until 2003 [18]. This local intervention was focused on GPs and paediatricians and aimed to improve the management of RTIs in children under the age of 6-years. Analysis of antibiotic prescribing data obtained from children’s health books showed a 50·0% reduction in the number of children receiving antibiotic prescriptions between 1999 and 2008. This reduction occurred despite no significant change in the average weekly number of RTI and bronchiolitis cases reported by GPs. Dommergues & Hentgen also found a 50·4% reduction in national annual antibiotic prescriptions within children aged under 18-years from 2001 to 2010, with the greatest reduction seen in children aged 0 to 24 months (57·2%) [21]. Although antibiotic prescribing rates have stabilised in recent years, Carlet et al. observed antibiotic prescribing rates remained 12·6% below baseline levels 14-years post-campaign [53].
The Belgium mass media campaign also used antibiotic prescribing data (defined daily doses per 1000 inhabitants per day (DID)) to show a significant impact from the campaign [19]. Following an initial decline of 12·1% from baseline to the end of the second campaign wave in 2007, prescribing rates fluctuated. However, the reduction in prescribing was maintained at 12·6% in 2018.
A pilot campaign in Egypt which aimed to raise awareness of rational antibiotic prescribing for RTIs among physicians, pharmacists, and the public used training courses to educate HCPs and social media to disseminate information within younger populations [48]. A 25·0 and 22·0% decline in antibiotic prescribing was seen post-intervention for children and adults respectively, with changes mainly being driven by reductions in prescribing for ear infections and bronchitis.
Studies evaluating the Canadian “Do Bugs Need Drugs” campaign reported inconsistent effects on antibiotic prescribing. Cumulative observed antibiotic use during the three years following the campaign implementation was 5·8% lower than expected values, with greater effects seen in the number of prescriptions dispensed to children (-10·6%) [23]. Furthermore, the effect on prescribing rates was dependent on the type of antibiotic and the condition for which the antibiotic was being prescribed [55].
Studies by Formoso et al. and Plachouras et al. used similar quasi-experimental study designs with campaigns implemented in specific regions with neighbouring provinces and national rates used as controls [23, 32]. Formoso et al. focused on antibiotic use in RTIs and used social marketing strategies to develop campaign messaging. Messaging was then disseminated via local media channels. Analysis of regional outpatient prescribing databases showed a significant 4.3% (95% CI: -7.1 to -1.5%) reduction in prescribing (DID) in intervention compared to control areas. Plachouras et al. relied on two-hourly education sessions for parents conducted by local HCPs and had limited use of the media to promote information. Within the Greek test regions antibiotic consumption was unchanged following the intervention and continued to follow trends seen nationally and within control regions.
A Slovenian campaign predominately aimed at HCP through educational workshops and the implementation of prescribing guidelines and restrictions, but with an element of public education in the form of flyers and posters on topics such as “The safe use of drugs” and “Get well without antibiotics” was implemented in 1995 [36]. Following an initial increase in prescribing rates of 3·97 DID from 1995 to 1999, antibiotic prescribing decreased resulting in a small net decrease of 5·0% since the campaign’s initiation.
Finally, a community campaign in 2018 which enrolled 21 clinics across ten locations in the USA also targeted HCPs through educational sessions and a cross-clinic comparison of prescribing data, with educational materials also provided to patients [25]. Assessment of the number of antibiotic prescriptions written for unresponsive RTIs showed a 46·0% reduction in prescribing post-intervention (OR: 0·54, 95% CI: 0·42 − 0·66, p = 0·001) after controlling for seasonality. However, this level of effect only occurred in two of the eleven clinics included in the study and no significant long-term intervention effect was evident.
Overall, a pooled analysis of the effect of European campaigns on DID’s suggest that implementation of a public campaign may reduce antibiotic consumption by 1·3 to 5·6 DID per 1,000 inhabitants [60].
Other outcome measures
Some campaign and intervention evaluations used other outcome measures. For example, campaign recognition and engagement were used by multiple studies evaluating the Antibiotic Guardian campaign. 26·5% of unique visitors to the Antibiotic Guardian campaign website made a pledge, 10·1% more than for a similar pledge-based campaign conducted in Sicily [29], with social media creating the greatest number of unique visitors to the Antibiotic Guardian website (29·0%) [61].
Similarities between campaigns reported to be effective
Evaluation of fourteen campaigns saw a significant improvement in their primary outcome measure, however there was a lack of homogeneity between these campaigns. Targeting a specific infection type (e.g. respiratory tract infection) was a common theme among campaigns that saw significant improvement in their primary outcome measure, these campaigns (n = 10) focused messages on the ineffectiveness of antibiotics at treating RTIs. Key messaging included “Antibiotics are not Automatic” [18, 21, 52,53,54], “Antibiotics are ineffective for common cold, acute bronchitis and flu” [19], “Antibiotics do not help in cold and flu” [22], and “Do Bugs Need Drugs” [24].
Mass media was used to disseminate messages in seven campaigns. The use of TV advertising to promote campaign messages was a recurring feature in mass media campaigns which saw a significant improvement in their primary outcome measure and was often cited as the main source of campaign recognition [19, 34, 38, 55]. Finally, some of these mass media campaigns which were reported as being effective also included an element of HCP education or promotion of HCP-patient interaction. This ranged from feedback to GPs on their antibiotic prescribing based on reimbursement data and facilitation of discussions between HCP and patients [19] to academic detailing, individual prescribing feedback and promotion of rapid streptococcal antigen tests [52] to promotional materials sent to all medical doctors and pharmacists [22], and accredited educational courses for physicians and pharmacists [24, 55].
A common theme among local and community interventions that saw a significant improvement in their primary outcome measure was an element of HCP education and using HCP-patient interactions to disseminate information. Part of the intervention implemented by Maor et al. included an explanation by physicians to parents for the reason their child has not been prescribed antibiotics during their visit [20]. Furthermore, Shehadeh et al. employed a similar method of disseminating information by employing pharmacists to provide ten-minute education sessions to the public on a one-to-one basis [46]. Finally, Kandeel et al. and Morgan et al. implemented HCP training programmes focusing on appropriate prescribing for RTIs for all clinical specialties, primary care doctors, as well as pharmacists and physicians working within outpatient clinics respectively [25, 48]. These training programmes were supplemented by educational resources targeting both HCPs, patients, and the public. Finally, the two remaining campaigns used school curriculum and social media combined with site-based resources to share campaign messaging regarding AMR and antibiotic use.
Campaign duration varied from 4 months [46] to 19-years [19] and did not seem predictive of significant improvements in the campaign evaluations primary outcome measure with only mass media campaigns repeated annually.
Discussion
Main findings
This review found some evidence suggesting national, community and local campaigns had a significant impact on the studies’ primary outcome measure. Knowledge and attitudes was the most used outcome measure to determine campaign effectiveness, followed by change in antibiotic prescribing rates. Most successful campaigns utilised mass media or HCP interaction with the public or patients to disseminate information. This suggests HCP interaction may be an important source of information or may mediate the pathway from knowledge acquisition to behaviour change in patients. However, further research is needed to gain a better understanding of the effect of HCP interaction on patient behaviours. Heterogeneity between studies made comparing the various public AMR campaigns and interventions challenging. It also created difficulties when drawing conclusions regarding the campaign components which are likely to contribute to a campaign’s success.
Only seven studies included in this review used a robust study design [23, 25, 32, 33, 36, 49, 56]. Five studies used a quasi-experimental or experimental study design combined with non-self-report outcome measures [23, 25, 32, 33, 36] which would enable the effectiveness of the campaign or intervention to be determined with a moderate level of validity and reliability [64]. Furthermore, while measurable outcomes, such as antibiotic prescribing and consumption, are informative due to their effect on AMR [65], few studies reported this in the context of GP consultation and RTI rates. Reporting of antibiotic prescribing rates in context provides information on whether the campaign has effectively raised awareness in the public or whether it has altered actions by HCP to ensure prescribing is appropriate. For campaigns with messaging focused on the self-limiting nature of RTIs, a reduction in consultations may suggest that public knowledge regarding infection prevention and the ineffectiveness of antibiotics at treating viral infections has improved. Antibiotic prescribing was reported in the context of GP consultations in studies evaluating the effectiveness of the 2001 French mass media campaign. Dunais et al. showed a significant reduction in prescribing despite no change in average weekly cases of RTI and bronchitis in under 5-year-olds reported by GPs. This indicates a reduction in prescribing for RTIs suggesting the addition of a local intervention aimed at GPs was more influential than the national mass media campaign aimed at improving public knowledge alone [18]. Chahwakilian et al. also found an initial 10·8% reduction in the proportion of consultations leading to a prescription. However, after four-years, the proportion of consultations resulting in an antibiotic prescription increased by 2·0%, suggesting latter declines in prescribing rates were mainly attributable to a continued decline in consultation rates [52]. This suggests campaign messaging encouraging self-care for RTI within the public was effective and long lasting, while aspects of the campaign aimed at inappropriate prescribing among GPs were less so. However, financial disincentives discouraging GP home visits for minor illness were introduced one-year into the campaign, in 2002, and is therefore likely to also have influenced consultation rates. Furthermore, comparisons made between studies evaluating the French national campaign should be interpreted with caution due to the differing data sources used to report on prescribing and consultation rates.
Findings from observational studies should be interpreted with caution due to potential confounding factors, such as other campaigns running concurrently, which limits our ability to assign impact to one specific campaign. Despite difficulties created when evaluating campaign effectiveness, multifaceted campaigns allow for multiple audiences to be targeted as was occurring in the UK between 2017 and 2019 where the Keep Antibiotics Working, Antibiotic Guardian and eBug campaigns and other HCP focused interventions [66, 67] were running simultaneously with significant improvements in AMR knowledge and awareness being reported by studies evaluating these campaigns.
Most studies only assessed the short-term impact of a campaign or intervention. Two exceptions are the evaluation of the long running mass media campaigns in France and Belgium. These campaigns both highlighted large initial reductions in antibiotic prescribing rates (34 and 10% respectively) following primary campaign waves which have subsequently increased, resulting in much smaller net reductions of 12·8% in Belgium and 12·6% in France [19, 53].
Previous research on general mass media health promotion campaigns concluded that short and long-term campaigns have similar levels of effectiveness [68]. This may be due to campaign fatigue resulting from long-term campaigns, causing inattention to campaign messaging, and therefore negatively impacting long-term behaviour change [69]. Therefore, further research is needed, especially in the area of AMR, to determine how to prevent campaign fatigue in the public, especially as health messaging currently saturates daily communication channels [70]. One such way to combat this is for campaigns to require active engagement, for example through making a pledge or interactive teaching sessions, rather than continuing to use static messaging to increase awareness as solely promoting awareness can be ineffective [35, 71]. The majority of included campaigns utilised predominately passive resources, such as TV advertising, posters, leaflets, and lectures from HCPs, with only four campaigns promoting interaction and engagement through pledge-based campaigns or interactive teaching sessions with children [29, 40, 61, 72]. However, those campaigns which have promoted engagement have only assessed change in AMR knowledge or self-reported behaviour which, while measuring the impact of the campaign more directly, makes it difficult to determine whether campaign engagement has led to actual behaviour change.
Future research
This review has highlighted several avenues for future research, primarily the need for a more standardised and robust approach to evaluating public health campaign effectiveness. The evaluation process needs to be considered and embedded within the initial design and development of the campaign with pre-determined outcome measures collected prior to and following the campaign; therefore, a campaign evaluation framework may be a beneficial tool for campaign developers to utilise. Some guidelines have been developed [73, 74] with one example being the ACME (audience–channel–message–evaluation) framework suggested by S. Noar (2012) which outlines key considerations regarding the audience, channel, messaging, and evaluation used when creating a public health campaign [75]. However, its real-world applicability may be limited due to changes in public health communication since its publication. One method which would allow standardised data to be collected on knowledge of AMR and appropriate antibiotic usage as well as antibiotic use behaviours is the implementation of national surveys which are conducted at regular intervals with examples being the tracking survey which is conducted in England and the Eurobarometer survey [76, 77]. As well as allowing for comparisons between countries, capturing this broader data on public knowledge of AMR and appropriate antibiotic usage would also allow differences in knowledge and behaviours between population groups to be determined, thus allowing campaign messaging or dissemination methods to be more targeted towards specific groups.
Furthermore, very few studies were identified which assessed campaign cost-effectiveness [19, 23, 36, 55], meaning it cannot be determined whether public health campaigns targeting AMR provide a good return on investment in terms of reduced cost of antibiotic prescriptions, reduced burden on HCPs or improved patient quality of life. Future research may wish to establish appropriate methods for conducting a cost-effectiveness analysis on AMR public health campaigns. Including these methods at the early stages of campaign design and development would add to the body of evidence assessing whether public health campaigns impact AMR. Building the body of evidence relating to the cost effectiveness of AMR public health campaigns is also likely to effect policy in this area as it may influence the availability of funding for future campaigns.
Finally, there have been a limited number of publications about campaigns conducted in recent years with only three campaigns launched in the last 5-years [25, 29, 49] and two ongoing campaigns [42, 61]. Methods of communication have changed substantially over recent years with the use of social media becoming increasingly prominent and it is now often cited as a preferred source of healthcare information for many [78]. However, this review highlighted only one study which piloted a social media focused campaign [31]. Furthermore, the majority of research on AMR messaging uses social media platforms which are no longer used extensively, such as Twitter [79], especially by younger populations who tend to have poorer knowledge of AMR and appropriate antibiotic usage [76, 80]. Social media and social media influencers have been shown to promote positive attitudes towards other health topics such as cervical screening [81]. As a result, future research may wish to explore the effectiveness of social media channels, such as Instagram, TikTok, Facebook and WhatsApp, as well as the use of influencers to disseminate information relating to AMR and appropriate antimicrobial usage, and to understand the volume of information and misinformation related to AMR which is available online.
Strengths and limitations
This review is the first to provide an overview of public health campaigns which aim to improve public knowledge of AMR and appropriate antibiotic use without restricting by research design. A strength of the study is the volume of papers screened, highlighting the broad range of campaigns which have been conducted globally. It also outlines some practical considerations that organisations can implement within their campaigns, namely, to ensure messaging is specific to a certain infection site, such as respiratory tract infections, that HCP education is considered alongside public education and that a mix of media sources are used to disseminate information. However, the review does have some limitations, mainly linked to the use of a rapid review methodology. Firstly, due to the rapid systematic review methodology, a limited number of databases were searched, however reference lists of previously conducted systematic reviews were reviewed and relevant papers extracted in an attempt to mitigate this. Also, the reference software was used to screen for articles containing key words relevant to review with only a subset of papers manually screened and a limited number of articles were screened by a second reviewer (4%). Finally, a quality assessment of included papers was not conducted, however this is not considered essential for rapid reviews, especially when scoping the available literature [82, 83], although any potential methodological issues have been highlighted within the narrative synthesis.
Conclusions
This review provides some evidence that evaluations of both large and small-scale campaigns reported significant improvements in outcome measures relating to AMR and antibiotic usage. Despite a lack of homogeneity between study designs some common themes emerged between effective campaigns, such as the use of mass media and HCP interaction to disseminate information, as well as the targeting of messaging towards a specific infection site, especially RTI.
However, the frequent use of observational study designs impacts the validity of their findings and makes it difficult to establish causation between the campaign and changes seen in the studies’ outcome measures. Furthermore, the lack of recently conducted campaigns creates difficulties when generalising findings to the public due to changes seen in health literacy following the COVID-19 pandemic. Finally, future work needs to identify a more standardised and robust approach to evaluating public health campaign effectiveness.
Data availability
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AMR:
-
Antimicrobial resistance
- CI 95%:
-
Confidence interval
- DID:
-
Defined daily dose per 100,000 inhabitants
- EAAD:
-
European Antimicrobial Awareness Day
- EU:
-
Europe
- GP:
-
General practitioner
- HCP:
-
Healthcare professional
- OR:
-
Odds ratio
- RTI:
-
Respiratory tract infections
- UK:
-
United Kingdom
References
Murray CJ, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet. 2022;399(10325):629–55.
Anderson M, et al. Averting the AMR crisis: what are the avenues for policy action for countries in Europe? 2019.
Van Rogers S, et al. Government policy interventions to reduce human antimicrobial use: a systematic review and evidence map. PLoS Med. 2019;16(6):e1002819.
Costelloe C, et al. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010;340:was 6.
UK Health Security Agency. English surveillance programme for antimicrobial utilisation and resistance (ESPAUR) - Report 2021 to 2022. 2022.
McKay R, et al. Systematic review of factors associated with antibiotic prescribing for respiratory tract infections. Antimicrob Agents Chemother. 2016;60(7):4106–18.
Fletcher-Lartey S, et al. Why do general practitioners prescribe antibiotics for upper respiratory tract infections to meet patient expectations: a mixed methods study. BMJ open. 2016;6(10):e012244.
Rather IA, et al. Self-medication and antibiotic resistance: crisis, current challenges, and prevention. Saudi J Biol Sci. 2017;24(4):808–12.
Anwar M, Iqbal Q, Saleem F. Improper disposal of unused antibiotics: an often overlooked driver of antimicrobial resistance. Expert Rev anti-infective Therapy. 2020;18(8):697–9.
Antwi A, Stewart A, Crosbie M. Fighting antibiotic resistance: a narrative review of public knowledge, attitudes, and perceptions of antibiotics use. Perspect Public Health. 2020;140(6):338–50.
Anastasi N, Lusher J. The impact of breast cancer awareness interventions on breast screening uptake among women in the United Kingdom: a systematic review. J Health Psychol. 2019;24(1):113–24.
Brown J, et al. How effective and cost-effective was the national mass media smoking cessation campaign ‘Stoptober’? Drug Alcohol Depend. 2014;135:52–8.
Cross ELA, Tolfree R, Kipping R. Systematic review of public-targeted communication interventions to improve antibiotic use. J Antimicrob Chemother. 2017;72(4):975–87.
Lim JM, et al. Impact of national interventions to promote responsible antibiotic use: a systematic review. J Antimicrob Chemother. 2020;75(1):14–29.
Moons P, Goossens E, Thompson DR. Rapid reviews: the pros and cons of an accelerated review process. Eur J Cardiovasc Nurs. 2021;20(5):515–9.
Richardson WS, et al. The well-built clinical question: a key to evidence-based decisions. Acp J Club. 1995;123(3):A12–3.
Fletcher-Miles H, Gammon J, Williams S, Hunt J. A scoping review to assess the impact of public education campaigns to affect behavior change pertaining to antimicrobial resistance. Am J Infect Control. 2020;48(4):433–42.
Dunais B, et al. Antibiotic prescriptions in French day-care centres: 1999–2008. Arch Dis Child. 2011;96(11):1033–7.
Bruyndonckx R, et al. Antibiotic use and resistance in Belgium: the impact of two decades of multi-faceted campaigning. Acta Clin Belg. 2021;76(4):280–8.
Maor Y, et al. Changing parents’ opinions regarding antibiotic use in primary care. Eur J Pediatrics. 2011;170:359–64.
Dommergues MA, Hentgen V. Decreased paediatric antibiotic consumption in France between 2000 and 2010. Scand J Infect Dis. 2012;44(7):495–501.
Ho ML, et al. Determinants of an effective antibiotic campaign: lessons from Hong Kong. J Global Antimicrob Resist. 2014;2(4):334–7.
Formoso G, et al. Feasibility and effectiveness of a low cost campaign on antibiotic prescribing in Italy: community level, controlled, non-randomised trial. BMJ. 2013;347.
Fuertes EI, et al. Trends in antibiotic utilization in Vancouver associated with a community education program on antibiotic use. Can J Public Health Revue Canadienne De Sante Publique. 2010;101(4):304–8.
Morgan BL, Bettencourt H, May L. Interrupted time-series analysis to evaluate the impact of a behavioral change outpatient antibiotic stewardship intervention. Antimicrob Stewardship Healthc Epidemiol. 2021;1(1):e37.
Adriaenssens N, et al. Implementation of e-Bug in Belgium. J Antimicrob Chemother. 2011;66 Suppl 5:pv51–3.
Koprivova Herotova T, Kostkova P, Benes J. e-Bug implementation in the Czech Republic. J Antimicrob Chemother, 2011;66 Suppl 5:v55–7.
Al-Mousa HH, Aly NY. Kuwait national campaign for proper use of antibiotics. Med Principles Pract. 2012;21(1):97.
Barchitta M, et al. The obiettivo antibiotico campaign on prudent use of antibiotics in Sicily, Italy: the pilot phase. Int J Environ Res Public Health. 2020;17(9):28.
Redding LE, Cole SD. Posters have limited utility in conveying a message of antimicrobial stewardship to pet owners. Front Veterinary Sci. 2019;6:(no pagination).
Zowawi HM, et al. The potential role of social media platforms in community awareness of antibiotic use in the Gulf cooperation council states: luxury or necessity? J Med Internet Res. 2015;17(10):e233.
Plachouras D, et al. Promoting prudent use of antibiotics: the experience from a multifaceted regional campaign in Greece. BMC Public Health. 2014;14:866.
van Rijn M, et al. The public uptake of information about antibiotic resistance in the Netherlands. Public Underst Sci. 2019;28(4):486–503.
Mazinska B, Struzycka I, Hryniewicz W. Surveys of public knowledge and attitudes with regard to antibiotics in Poland: did the European antibiotic awareness day campaigns change attitudes? PLoS ONE. 2017;12(2):e0172146.
Lawrence C, Ferguson E. Public health messages about antibiotic treatment for respiratory tract infection may increase perceived symptom severity reporting. J Health Psychol. 2019;24(5):623–7.
Fürst J, et al. The influence of a sustained multifaceted approach to improve antibiotic prescribing in Slovenia during the past decade: findings and implications. Expert Rev anti-infective Therapy. 2015;13(2):279–89.
Chaintarli K, et al. Impact of a United Kingdom-wide campaign to tackle antimicrobial resistance on self-reported knowledge and behaviour change. BMC Public Health. 2016;16:393.
UKHSA., English surveillance programme for antimicrobial utilisation and resistance (ESPAUR). Report 2020 to 2021. 2021.
McNulty CA, et al. The English antibiotic awareness campaigns: did they change the public’s knowledge of and attitudes to antibiotic use? J Antimicrob Chemother. 2010;65(7):1526–33.
Allison DG, Higginson P, Martin S. Antibiotic resistance awareness: a public engagement approach for all pharmacists. Int J Pharm Pract. 2017;25(1):93–6.
Foo YL, et al. Understanding the use of antibiotics and antibiotic resistance among science stream and non-science stream undergraduate students in a Malaysian University. J Liaquat Univ Med Health Sci. 2021;20(5):350–7.
Hayes C, et al. International promotion of e-Bug, an infection prevention and control educational intervention: survey of partners across 14 countries. JAC Antimicrob Resist. 2020;2(1).
UK Health Security Agency. English surveillance programme for antimicrobial utilisation and resistance (ESPAUR) - Report 2020 to 2021. 2021.
Thong KS, et al. Impact of targeted educational intervention towards public knowledge and perception of antibiotic use and resistance in the state of Perak, Malaysia. Antimicrob Resist Infect Control. 2021;10(1):29.
Phueanpinit P, et al. Knowledge and perceptions of outpatients regarding upper respiratory tract infections and awareness of an antibiotics smart use campaign in Thailand. J Pharm Pract Res. 2022;52(4):294–302.
Shehadeh MB, Suaifan GA, Hammad EA. Active educational intervention as a tool to improve safe and appropriate use of antibiotics. Saudi Pharm J. 2016;24(5):611–5.
Ngadimon IW, et al. Improving shared decision-making in adolescents through antibiotic education. Int J Clin Pharm. 2017;39(1):120–5.
Kandeel A, et al. An educational intervention to promote appropriate antibiotic use for acute respiratory infections in a district in Egypt- pilot study. BMC Public Health. 2019;19(Suppl 3):498.
Khoshgoftar M, et al. The effect of public health educational campaign regarding antibiotic use and microbial resistance on knowledge, attitude, and practice in the Iran. J Educ Health Promotion. 2021;10:3.
Newitt S, et al. Expansion of the ‘Antibiotic Guardian’ one health behavioural campaign across Europe to tackle antibiotic resistance: pilot phase and analysis of AMR knowledge. Eur J Pub Health. 2018;28(3):437–9.
Newitt S, et al. Demographic, knowledge and impact analysis of 57,627 antibiotic guardians who have pledged to contribute to tackling antimicrobial resistance. Antibiotics. 2019;8(1):09.
Chahwakilian P, et al. Impact of the French campaign to reduce inappropriate ambulatory antibiotic use on the prescription and consultation rates for respiratory tract infections. J Antimicrob Chemother. 2011;66(12):2872–9.
Carlet J, et al. Trends in antibiotic consumption and resistance in France over 20 years: large and continuous efforts but contrasting results. Open Forum Infectious Diseases. 2020;7(11).
Bernier A, et al. Outpatient antibiotic use in France between 2000 and 2010: after the nationwide campaign, it is time to focus on the elderly. Antimicrob Agents Chemother. 2014;58(1):71–7.
McKay RM, et al. Evaluation of the do bugs need drugs? Program in British Columbia: can we curb antibiotic prescribing? Can J Infect Dis Med Microbiol. 2011;22(1):19–24.
Munoz EB, et al. The effect of an educational intervention to improve patient antibiotic adherence during dispensing in a community pharmacy. Aten Primaria. 2014;46(7):367–75.
Kesten JM, et al. The antibiotic guardian campaign: a qualitative evaluation of an online pledge-based system focused on making better use of antibiotics. BMC Public Health. 2017;18(1):5.
Mazinska B, Hryniewicz W. European antibiotic awareness day educational campaign–has it changed public attitudes to antibiotic use in Poland?. Polski Merkuriusz Lekarski. 2010;29(173):296–303.
Maor Y, et al. Changing parents’ opinions regarding antibiotic use in primary care. Eur J Pediatrics. 2011;170(3):359–64.
Filippini M, Ortiz LG, Masiero G. Assessing the impact of national antibiotic campaigns in Europe. Eur J Health Econ. 2013;14(4):587–99.
Bhattacharya A, et al. A process evaluation of the UK-wide antibiotic guardian campaign: developing engagement on antimicrobial resistance. J Public Health. 2017;39(2):e40–7.
Borgonha A. Communicating antibiotic resistance to the public. How effective was public health England’s 2018 ‘Keep antibiotics working’ campaign TV advertisement at increasing public understanding of antibiotic resistance and motivating a change in antibiotic seeking behaviours? 2019.
Commission E. Special eurobarometer 445 report antimicrobial resistance 2016. 2016.
Rogers J, Revesz A. Experimental and quasi-experimental designs. Routledge; 2020.
Bell BG, et al. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infect Dis. 2014;14(1):1–25.
Anyanwu PE, et al. Investigating the mechanism of impact and differential effect of the quality premium scheme on antibiotic prescribing in England: a longitudinal study. BJGP Open. 2020;4(3).
Jones LF, et al. An evaluation of the TARGET (Treat Antibiotics Responsibly; Guidance, Education, Tools) antibiotics toolkit to improve antimicrobial stewardship in primary care-is it fit for purpose? Fam Pract. 2018;35(4):461–7.
Quattrin R, Filiputti E, Brusaferro S. Health promotion campaigns and mass media: looking for evidence. Prim Health Care: Open Access. 2015;5(1):1–7.
So J, Kim S, Cohen H. Message fatigue: conceptual definition, operationalization, and correlates. Communication Monogr. 2017;84(1):5–29.
Kim S, So J. How message fatigue toward health messages leads to ineffective persuasive outcomes: examining the mediating roles of reactance and inattention. J Health Communication. 2018;23(1):109–16.
Hill MD, Thompson-Hayes M. From awareness to commitment in public health campaigns: the awareness myth. Rowman & Littlefield; 2017.
McNulty CA, et al. Overview of e-Bug: an antibiotic and hygiene educational resource for schools. J Antimicrob Chemother. 2011;66:v3–12.
Service GC, Guide to campaign planning: OASIS, service GC. Editor. 2020. https://gcs.civilservice.gov.uk/guidance/marketing/delivering-government-campaigns/guide-to-campaign-planning-oasis/
Trust W. Reframing Resistance. 2019. https://wellcome.org/reports/reframing-antimicrobial-resistance-antibiotic-resistance
Noar SM. An audience–channel–message–evaluation (ACME) framework for health communication campaigns. Health Promot Pract. 2012;13(4):481–8.
McNulty CA, Collin SM, Cooper E, Lecky DM, Butler CC. Public understanding and use of antibiotics in England: findings from a household survey in 2017. BMJ Open. 2019;9(10):e030845.
European Centre for Disease Prevention and Control. Survey of healthcare workers’ knowledge, attitudes and behaviours on antibiotics, antibiotic use and antibiotic resistance in the EU/EEA. LU: Publications Office. 2019 Feb 23.
Frey E, et al. Parents’ use of social media as a health information source for their children: a scoping review. Acad Pediatr. 2022;22(4):526–39.
Andersen B, et al. Understanding and diagnosing antimicrobial resistance on social media: a yearlong overview of data and analytics. Health Commun. 2019;34(2):248–58.
Volkmer I. Social media and COVID-19: A global study of digital crisis interaction among Gen Z and millennials. 2021.
Fielden N, Holch P. Exploring the influence of social media influencers on intention to attend cervical screening in the UK: utilising the theory of planned behaviour. Cancer Control. 2022;29:10732748221079480.
Haby MM, Chapman E, Clark R, Barreto J, Reveiz L, Lavis JN. What are the best methodologies for rapid reviews of the research evidence for evidence-informed decision making in health policy and practice: a rapid review. Health Res Policy Syst. 2016;14(1):1–2.
Tricco AC, Langlois E, Straus SE. World Health Organization. Rapid reviews to strengthen health policy and systems: a practical guide. World Health Organization; 2017.
Acknowledgements
We acknowledge the members of the UKHSA insights for AMR campaigns group: Anna Flanagan, Dale Weston, Gillian Hayes, Rose Hadden, Donna Lecky, Russell Hope, Joanna Conneely, Diane Pople, Julie Robotham, Eleanor Harvey and Colin Brown. We also acknowledge Mary Jordan, University of Warwick, and Connie Longmate, Department of Health and Social Care.
Funding
No specific funding was provided for this study.
Author information
Authors and Affiliations
Contributions
Conceptualisation: DAO, EG, VC; methodology: DAO, EG, NPS; original draft: EG, NPS, DAO; validation: DAO, VC, NPS. All authors have read and agreed to the final draft.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
DAO is the lead for the Antibiotic Guardian campaign; all other authors declare no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1:
PRISMA 2020 item checklist. Supplementary Material 2. Search Strategies
Supplementary Material 2:
Search Strategies
Supplementary Material 3:
PRISMA diagram outlining the study selection process
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gilham, E.L., Pearce-Smith, N., Carter, V. et al. Assessment of global antimicrobial resistance campaigns conducted to improve public awareness and antimicrobial use behaviours: a rapid systematic review. BMC Public Health 24, 396 (2024). https://doi.org/10.1186/s12889-024-17766-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-17766-w