- Research
- Open access
- Published:
Descriptive study of foodborne disease using disease monitoring data in Zhejiang Province, China, 2016–2020
BMC Public Health volume 22, Article number: 1831 (2022)
Abstract
Background
This study aimed to identify the epidemiology, seasonality, aetiology and clinical characteristics of sporadic foodborne diseases in Zhejiang province during 2016–2020.
Methods
Descriptive statistical methods were used to analyze the data from surveillance network established by the Zhejiang Provincial Center for Disease Control and Prevention. There were 31 designated hospitals in all 11 cities which were selected using probability proportionate to size sampling method.
Results
During the study period, the surveillance system received 75,124 cases with 4826 (6.42%) hospitalizations from 31 hospitals. The most common cause was Norovirus, 6120 cases (42.56%), followed by Salmonella, 3351 cases (23.30%). A significant seasonal trend was observed for the V. parahaemolyticus, with the highest rates over the summer period, peaking in August, 1171 cases (38.75%), a similar trend was also observed with Salmonella and Diarrheagenic E. coli. Norovirus infections showed the highest rate in November (904, 14.77%) and March (660,10.78%), the lowest in August, 215 cases (3.51%). Patients between 19 ~ 40 years were more likely to infected by Norovirus, V. parahaemolyticus and Diarrheagenic E. coli, patients below 1 year were the highest among patients with Salmonella infection, 881 cases (26.3%). The Norovirus, V. parahaemolyticus and Diarrheagenic E. coli infection with the highest positive detection rates among the workers were observed. The largest number cases of food categories were from aquatic product infection. The private home was the most common exposure setting.
Conclusion
Our study highlighted the necessity for conducting an active, comprehensive surveillance for pathogens in all age groups, to monitor the changing dynamics in the epidemiology and aetiology of foodborne diseases to guide policies that would reduce related illnesses.
Introduction
Foodborne illnesses are usually infectious or virulent and caused by bacteria, viruses, parasites or chemicals that enter the body through contaminated food or water. Although, food science and related technologies are developing rapidly, but still, it remains a challenge to prevent foodborne diseases completely [1]. An estimated 600 million in the world (almost 1 in 10 people), fall ill after eating contaminated food and 420 000 die every year, resulting in the loss of 33 million healthy life years in terms of Disability Adjusted Life Years (DALYs) according to an estimate based on the 2015 data [2]. Diarrhoeal diseases account for more than 50% of foodborne diseases, according to the data released by World Health Organization (WHO), foodborne or water-borne diarrhea alone causes about 2.2 million deaths worldwide every year [3]. As in other countries, foodborne diseases characterized by acute gastrointestinal diseases are the largest food safety problem as well as the most distressing food-related threat to public health in China [4,5,6]. In order to reduce the disease burden, China has established a web-based foodborne disease surveillance system since 2011, which has gradually played a role in food safety incidence prevention. The surveillance contents include hygiene indicator bacteria, pathogenic bacteria, viruses, and parasites in many food categories. Moreover, sampling points are no more limited to retail and catering sites, and have been extended to processing, and sales locations.
The studies discussed the characteristics of food contamination by pathogens according to surveillance data and reflects the contamination and distribution trend of foodborne pathogens in different regions. A wide range of representative agents (including pathogenic bacteria, viruses and etc.) are covered to understand their contamination in meat and meat products [7], milk and dairy products [8], eggs and egg products [9], children’s foods [10] and ready-to-eat foods [11]. Norovirus, Salmonella spp., Vibrio parahaemolyticus (V. parahaemolyticus), Shigella and Diarrheagenic E. coli have been identified as the most common pathogens responsible for foodborne diseases in China [12, 13]. The surveillance data showed that occurrence of V. parahaemolyticus in aquatic products tended to increase over the period from 2015 to 2018 [11, 14].
Safe food supplies support national economies, trade and tourism, contribute to food and nutrition security, and underpin sustainable development. As there are a limited number of existing epidemiological studies and reports on the foodborne diseases in Zhejiang province, the need for researches has become important. The aim of this study was to summarize epidemiological characteristics of foodborne disease cases and provide effective interventions to prevent foodborne disease illnesses in Zhejiang province, we analyzed the surveillance data of foodborne disease cases caused by Norovirus, Salmonella spp., Vibrio parahaemolyticus (V. parahaemolyticus), Shigella and Diarrheagenic E. coli in Zhejiang province from 2016 to 2020.
Methods
Geographical position, climatic and socio-demographic feature of study site
Zhejiang Province, one of the southeastern coastal provinces of China, is located at 27°02’N to 31°11’N and 118°01’E to 123°10’E [15], the 11 cities and their subordinate counties are listed in Supplementary Table 1. Zhejiang experience a subtropical humid climate. During summer the weather is hot and humid and the temperature is around 27 to 30 °C (81 to 86 °F). During winter the temperature falls down to a minimum temperature of 2℃ to 8℃ (36 to 46 °F). Rainfall and typhoons are a common phenomenon in summers. Zhejiang province has a permanent population of 65.4 million at the end of 2021, and GDP grew 8.5% year-on-year to 7.35 trillion yuan ($1.16 trillion) in 2021 [15]. Most of Zhejiang’s wealth derives from light industry and mostly located in rural villages [16].
Data source
Zhejiang Provincial Center for Disease Control and Prevention (ZJCDC) has collected foodborne disease relevant data through the China National Foodborne Diseases Surveillance Network (NFDSN) since 2012. 31 hospitals were inquired to detect 5 major pathogens and corresponding subtypes, including Salmonella, Norovirus, V. parahaemolyticus, Diarrheagenic E. coli and Shigella for all suspected foodborne disease cases, and reported illnesses through NFDSN since 2016. In this study the cases reported by 31 hospitals in Zhejiang province during the period 2016–2020 were included. Epidemiologists from the health departments first conducted the investigation to ascertain the full extent of the foodborne illness and the information collected for each case includes reporting region, date of occurrence, setting, etiology, food categories, number of illnesses / hospitalizations, and some other details. Unknown etiology refers to those foodborne disease cases where the confirmed etiology has not been identified. Foods was identified as the sources of disease through epidemiologic or laboratory methods and was classified into 13 categories. The food that cannot be determined was classified as “Unknown”. The GIS map data of Zhejiang Province is downloaded by the national basic geographic information center of China (http://bzdt.ch.mnr.gov.cn/).
Statistical analysis
Total positive detection rate and hospitalization rate were calculated for each pathogen and linear trend test was used to test the change of positive detection rate and hospitalization rate annually for each pathogen. Chi-square test was used to compare the demographic characteristics, contaminated food category and food settings among four pathogens, including Salmonella, Norovirus, V. parahaemolyticus, Diarrheagenic E. coli while Shigella was not included due to limited sample sizes. Fisher exact test was used if the conditions were not met for Chi-square test. Post-hoc test was used for pairwise comparisons. Comparison was only programmed within illnesses with single etiology. Open-source software QGIS (Quantum GIS version 3.22.9) was used to map the spatial distribution of cases with positive detection rate caused by five pathogens for the period between 2016 and 2020. All statistical analyses were performed using R 3.6.2 and P-value was considered as significant at < 0.05.
Results
General epidemiological characteristics
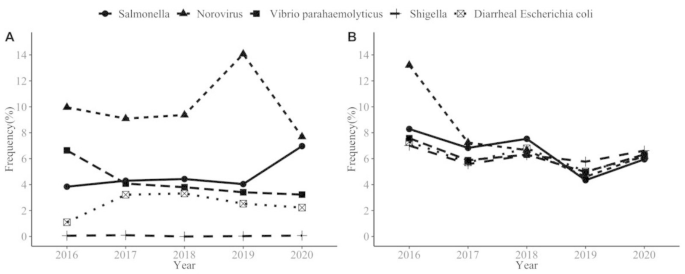
During the study period (2016–2020), the surveillance system received 75,124 cases with 4826 (6.42%) hospitalizations from 31 hospitals. As shown in Table 1, total positive detection rate was 14,381(3.97%). The most common cause was Norovirus, 6120 cases (42.56%), followed by Salmonella, 3351 cases (23.30%), V. parahaemolyticus, 3022 cases (21.01%), Diarrheagenic E. coli,1849 cases (12.86%) and Shigella, 39 cases (0.27%). The positive detection rate increased in Salmonella and E. coli (from 3.37 to 6.59% and from 1.14 to 2.38%, respectively), while the rate for V. parahaemolyticus and Norovirus decreased during 2016–2020 (from 6.29 to 2.39% and from 10.62 to 6.62%, respectively); the rate in Shigella remained low level (Fig. 1.A). As for hospitalization rate, a significant decrease of Norovirus and Salmonella was observed during the study period as well (P < 0.001), with the highest in 2016 (from 12.62 to 6.55% and from 8.21 to 6.24%, respectively) (Fig. 1.B). Among all cases with positive detection, which were being hospitalized, the most common cause was Salmonella (Table 1).
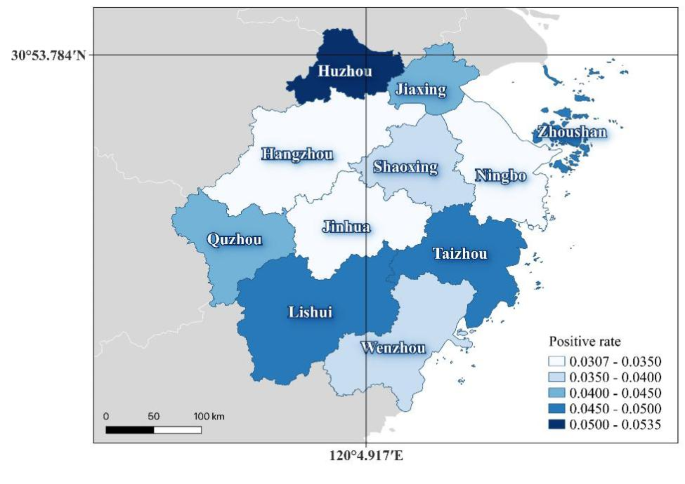
The regional distribution of cases with positive caused by five pathogens among 11 cities, as shown in Fig. 2: 2028 cases with 5.34% detection rate in Huzhou city, 1636 (4.89%) cases in Taizhou city, 1073 (4.88%) cases in Lishui city (Fig. 2).
Characteristics for four pathogens
For this analysis, only the highest contributing pathogens were included (Salmonella, Norovirus, V. parahaemolyticus, and Diarrheagenic E. coli).
Trend and seasonality
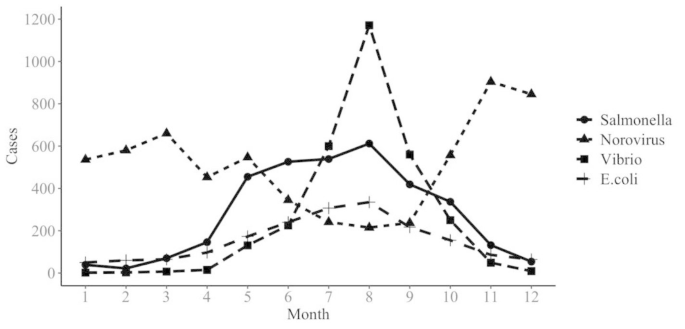
A significant seasonal trend was observed for the V. parahaemolyticus, with the highest rates over the summer period, peaking in August, 1171 cases (38.75%). A similar trend was also observed with Salmonella and Diarrheagenic E. coli, with the peak in August, 612 cases (18.26%) and 335 cases (18.12%), respectively. Norovirus infections showed the highest rate in November (904 cases, 14.77%) and March (660 cases,10.78%) and the lowest in August, 215 cases (3.51%) (Fig. 3).
Age, gender and occupational differences
A significant difference was observed between different age groups (P < 0.01), with the majority of reported cases affecting young people aged 19–40 years, as shown in Table 2. Among Salmonella infections, illnesses below one year old accounted for 26.30%, significantly higher than other three pathogens. V. parahaemolyticus showed much lower proportion for illnesses in population under 18 years old. As for gender distribution, though significantly different among four pathogens, all showed higher proportion in males (P < 0.05). A significant occupational difference was observed. For Norovirus, V. parahaemolyticus and Diarrheagenic E. coli infection with the highest proportion among the workers. Salmonella infections showed the highest proportion in kids living scattered,1180 cases (35.21%) (Table 2).
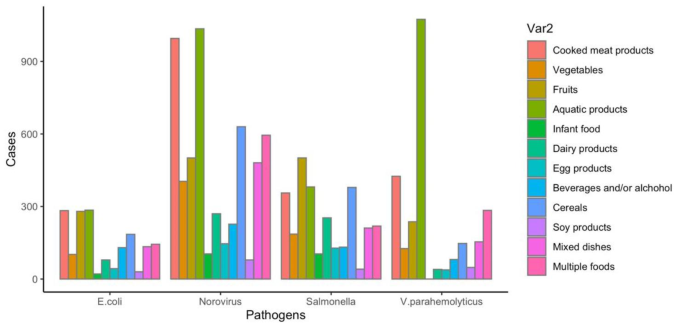
Implicated foods and settings
In this study, four type of foodborne cases were reported due to certain food vehicles, as shown in Fig. 4. Aquatic products were the most common cause for Norovirus, V. parahaemolyticus and Diarrheagenic E. coli infection (17.73%, 39.34% and 15.84%, respectively), followed by cooked meat products (17.04%, 15.57% and 15.73% respectively). The top three food vehicles in Salmonella infection were fruits (16.25%), aquatic products (12.36%) and cereals (12.29%). The places with more cases caused by four pathogens were household settings, followed by restaurants, data shown in Table 3.
Symptoms
Among the Norovirus cases: 52.81% with abdominal cramps, 38.35% with vomiting, 38.28% with nausea; Salmonella caused 49.93% abdominal cramps, 28.20% fever, 19.04% nausea cases; V. parahaemolyticus caused 76.15% abdominal cramps, 46.92% nausea, 37.62% vomiting cases; Diarrheagenic E. coli caused 60.57% abdominal cramps, 25.26% nausea, 19.47% vomiting cases. Watery diarrhea was the most common symptom for four pathogens (Table 4).
Discussion
Foodborne diseases impede socioeconomic development by straining health care systems, and harming national economies, tourism and trade. This study described the epidemiology of foodborne diseases caused by different pathogens in Zhejiang Province during the period 2016–2020. Over the 5 years, 75,124 cases with 4826 (6.42%) hospitalizations caused by Norovirus, Salmonella, V. parahaemolyticus, Diarrheagenic E. coli and Shigella from 31 hospitals were reported. Among 11 cities, 2028 cases in Huzhou city (14.33%), 1933 cases in Wenzhou city (13.66%), 1636 cases in Taizhou city (11.56%). The results were quite different from Sun Liang’s report, in which Wenzhou city accounts for the largest percentage of illnesses [17].
The number of illnesses caused by Norovirus ranks first among all etiologies, which is consistent with Shanghai, in which Norovirus was the most common pathogen (43.10%) [18], but quite different from the studies in China’s coastal provinces such as Hainan [19]. Wang [20] et al. reviewed 2447 papers in China that reported 1082 foodborne disease cases occurring between 1994 and 2005, in which V. parahaemolyticus caused the most events in littoral provinces, whereas in inland provinces, the largest percentage of cases were caused by Salmonella. Thus, there are regional differences in the distribution of pathogenic bacteria in China. These studies suggests that region-specific policies on foodborne disease control should be established.
Seasonality of foodborne illnesses was observed in this study. A seasonal trend was found for the V. parahaemolyticus, Salmonella and Diarrheagenic E. coli with the highest rates during summer period, peaking in August, this was similar in Enserink’s [21] and Gong’s [18] reports. However, the seasonal peak of infection attributed to some foodborne pathogens isn’t in the summer. For instance, Norovirus infections showed the highest rate in November and March and the lowest in summer, which was in line with previous studies [18, 22, 23]. Seasonality related to the temperature, humidity and rainfall, all of which may affect exposure frequency and host immune status. These findings indicated that temperature is an important factor in foodborne illnesses, and investigation of the reasons for the seasonal dominance on foodborne diseases should be the focus of surveillance.
This study showed the distinctive differences between four main pathogens with age groups. In general, the positive detection rate was higher in people aged 19 ~ 30 and 31 ~ 40 years than that in those aged < 18 and 40 + years, which were infected by Norovirus, V. parahaemolyticus and Diarrheagenic E. coli. This was partly consistent with a study in China which found incidence of foodborne diseases in youth group was higher than that in elderly group [14]. Also, a study in France which found incidence of foodborne diseases in young was higher than that in elders, in which, elders (≥ 60 years) were at least likely to get infected with V. parahaemolyticus, whereas people aged 30 ~ 44 years were the most likely get infected [24]. Similar results were observed in a Shanghai study [25]. In contrast to previous studies which found children (< 5 years) and elder people more likely to get infected with Norovirus [26, 27], our study found that the highest proportion in Norovirus infections was people aged 19–30 years old. Among Salmonella infections, cases among children aged under 1 year old accounted for 26.30%, significantly higher than other age groups. Similar findings reported in Guangdong Province that children aged < 5 years were the group most affected by Salmonella (73%), of whom the infants under 1 year old were 81.5% [28]. As for gender distribution, though significantly different among four pathogens, all showed higher proportion in male. The Norovirus, V. parahaemolyticus and Diarrheagenic E. coli infection with the highest positive detection rates in the workers were observed. Foodborne illnesses among workers are liable to occur frequently because poor hygienic conditions at workers’ camps and work situations, in the meantime, high summer temperatures impacting the transportation, distribution and storing of foods [29]. The related knowledge on what is safe should be handed down through families, work sites and credible institutions.
Analysis of exposed foods of foodborne illnesses in this study, the cases caused by Norovirus, V. parahaemolyticus and Diarrheagenic E. coli, the largest number of food categories involved were aquatic product infection (17.73%, 39.34% and 15.84%, respectively). On the contrary, a study showed the analysis of exposed foods of reported cases in Shandong Province, multiple foods (meaning more than two kinds of food) were the most commonly reported classification [30]. The reason for the different findings may be that Zhejiang is a coastal province with a vast sea area and various aquatic products. Therefore, consumers would be advised to separate raw and cooked foods, cook thoroughly as much as possible and keep food at safe temperatures to reduce the risk of foodborne diseases. However, avoiding all raw seafood should be difficult for those who are in the habit of eating seafood. As for cases infected by Salmonella, fruits, aquatic products and cooked meat products were identified as the most frequent food vehicles in the present study. Conversely, eggs have been reported as the most common classification for Salmonella infection in the US [31]. The main reason for this difference was cultural differences in eating habits. Yet it’s worth noting that, the reported classification of multiple foods relatively high as well. That means people eat more and more diverse foods, on the other hand, the category of exposed foods in national foodborne disease surveillance system is not specified in enough detail.
Analysis of the settings, according to our analysis, private home was the most common exposure setting, followed by restaurant. However, the average annual case ratios in the Republic of Korea were the highest at restaurant (57%) [32]. Among cases reported in US, restaurants also the most common settings of preparation [31]. On the contrary, Wu et al. [33] from CDC of China found that, foodborne illnesses most frequently occurred in household (32%). Similar results were observed in a EU study [34]. These findings consistent with present results, this means a large proportion of foodborne diseases caused by foods improperly prepared or mishandled at home. The effective actions can include the following aspects: know the food they use, for example, read labels on food packages, make informed choices, become familiar with common food hazards; furthermore, government should focus on home settings to reduce infections.
In regard to clinical symptoms in general, results showed similar clinical symptoms, such as nausea, abdominal pain and watery diarrhea between patients caused by four pathogens, respectively. The proportion of fever was the highest in Salmonella while lowest in Diarrheagenic E. coli. The proportion of fever in Salmonella infections in our findings was close to that in another research [35]. As Most foodborne pathogens can cause acute gastroenteritis with gastrointestinal symptoms, it is difficult to distinguish the cases infected by different pathogens by symptoms.
The limitations of this study need to be explained. First, for many reported cases, information on certain aspects, such as food category, settings and etc. were missing or incomplete, so the conclusions might not be representative of unknown classifications. Second, information and detection data were collected from 31 hospitals and several laboratories. Though detection methods were unified and regular trainings were held, there was a chance of bias caused by the different conditions and levels of hospitals and laboratories. Third, inability to conduct an epidemiological investigation due to lack of patient cooperation, there were still some missing information.
Conclusion
Norovirus was the most common enteric pathogen detected in our surveillance during 2016–2020. Since the different epidemiological characteristics of foodborne diseases caused by different pathogens, we suggest that targeted measures be taken according to the characteristics of different etiologies and food vehicles to improve the prevention and control efficiency. The Norovirus, V. parahaemolyticus and Diarrheagenic E. coli infection with the highest positive detection rates over the workers were observed. Foodborne illnesses among workers are liable to occur frequently because hygienic conditions at workers’ camps and work situations are not always at the same standard. The related knowledge on what is safe should be handed down through families, work sites and credible institutions. Most foodborne diseases are preventable, we should further improve the identification rate of the causes of the epidemic, carry out attribution analysis for “precise prevention and control”.
Data availability
The data that support the findings of this study are available from the Foodborne Disease Case Surveillance Reporting System of the China National Center for Food Safety Risk Assessment, and these data are not publicly available.
The data that support the findings of this study are available from the Foodborne Disease Case Surveillance Reporting System (https://sppt.cfsa.net.cn/goto), and these data are not publicly available.
References
Kim JJ, Ryu S, Lee H. Foodborne illness outbreaks in Gyeonggi province, Korea, following seafood consumption potentially caused by Kudoa septempunctata between 2015 and 2016. Osong Public Health Res Perspect. 2018;9:66–72.
World Health Organization. WHO estimates of the global burden of foodborne diseases: foodborne diseases burden epidemiology reference group 2007–2015. https://www.who.int/publications/i/item/9789241565165. Accessed 3 December 2015.
Food Standards Agency. The FSA food borne disease strategy 2010-15. London: Food Standards Agency; 2011.
Chung SS, Wong CK. Regulatory and policy control on food safety in China. J Epidemiol Community Health. 2013;67(6):476–7.
Akhtar S, Sarker MR, Hossain A. Microbiological food safety: a dilemma of developing societies. Crit Rev Microbiol. 2014;40(4):348–59.
Wu YN, Liu P, Chen JS. Food safety risk assessment in China: Past, present and future. Food Control. 2018;90:212–21.
Yang S, Yan L, Pei X, Yang D. Study on the contamination status of foodborne pathogens in frozen minced meat products on China market. Chin J Food Hyg. 2020;32:180–3.
Yan L, Li Y, Yang D, et al. Contamination of pathogens in milk powder available in retail markets. Chin J Public Health. 2016;32:602–4.
Li Y, Yang X, Zhang H, et al. Prevalence and antimicrobial susceptibility of Salmonella in the commercial eggs in China. Int J Food Microbiol. 2020;325:108623.
Hu J, Pei X, Li N, Yang D. Survey of microbiological contamination of commercial available infant formula sheep milk powder. Chin J Health Lab Tec 2016;26:1942–1943, 1946.
Kim HW, Hong YJ, Jo JI, et al. Raw ready-to-eat seafood safety: microbiological quality of the various seafood species available in fishery, hyper and online markets. Lett Appl Microbiol. 2017;64(1):27–34.
Li W, Cui Q, Bai L, Fu P, Han H, Liu J, Guo Y. Application of Whole-Genome Sequencing in the National Molecular Tracing Network for Foodborne Disease Surveillance in China. Foodborne Pathog Dis. 2021;18(8):538–46.
Kim SS, Kang DH. Combination treatment of ohmic heating with various essential oil components for inactivation of food-borne pathogens in buffered peptone water and salsa. Food Cont. 2017;80:29–36.
Yan L, Hu J, Pei X, Yang D, Zhang X. Contamination of foodborne pathogens in frozen surimi products sold in China in 2014. J Hyg Res. 2017;46:328–30.
Zhejiang Provincial Bureau of Statistics. http://tjj.zj.gov.cn/.
Official site of Zhejiang province. China. http://www.ezhejiang.gov.cn/index.html.
Sun L, Chen Ll, Liao NB, Chen J. Analysis of foodborne disease outbreak surveillance data in Zhejiang Province,2006–2017. Chin J Health Lab Tec. 2019;29(15):1874–7.
Gong XH, Wu HY, Li J, Xiao WJ, Zhang X, Chen M, Teng Z, Pan H, Yuan ZA. Epidemiology, aetiology and seasonality of infectious diarrhoea in adult outpatients through active surveillance in Shanghai, China, 2012–2016: a cross-sectional study. BMJ Open. 2018;8(9):e019699.
Wang JX, He J, Wang S, et al. Incidence of foodborne diseases in Hainan province, 2007–2016. Chin J Public Health. 2018;34(9):1288–91.
Wang S, Duan H, Zhang W, Li JW. Analysis of bacterial foodborne disease outbreaks in China between 1994 and 2005. FEMS Immunol Med Microbiol. 2007;51(1):8–13.
Enserink R, van den Wijngaard C, Bruijning-Verhagen P, et al. Gastroenteritis attributable to 16 enteropathogens in children attending day care: significant effects of rotavirus, norovirus, astrovirus, Cryptosporidium and Giardia. Pediatr Infect Dis J. 2015;34(1):5–10.
Karsten C, et al. Incidence and risk factors for community-acquired acute gastroenteritis in north-west Germany in 2004. Eur J Clin Microbiol Infect Dis. 2009;28(8):935–43.
Zhang Z, Lai S, Yu J, et al. Etiology of acute diarrhea in the elderly in China: A six-year observational study. PLoS ONE. 2017;12(3):e0173881.
Arena C, Amoros JP, Vaillant V, et al. Acute diarrhea in adults consulting a general practitioner in France during winter: incidence, clinical characteristics, management and risk factors. BMC Infect Dis. 2014;14:574.
Zhang Y, Zhao Y, Ding K, Wang X, Chen X, Liu Y, Chen Y. Analysis of bacterial pathogens causing acute diarrhea on the basis of sentinel surveillance in Shanghai, China, 2006–2011. Jpn J Infect Dis. 2014;67(4):264–8.
Hossain ME, Islam MM, Miah M, Haque W, Vinjé J, Rahman MZ, Faruque ASG, Khan AI, Ahmed T, Rahman M. Corrigendum to: Viral Etiology of Acute Gastroenteritis Among Forcibly Displaced Myanmar Nationals and Adjacent Host Population in Bangladesh. J Infect Dis. 2022;225(6):1114.
Patel MM, Widdowson MA, Glass RI, Akazawa K, Vinjé J, Parashar UD. Systematic literature review of role of noroviruses in sporadic gastroenteritis. Emerg Infect Dis. 2008;14(8):1224–31.
Liang Z, Ke B, Deng X, Liang J, Ran L, Lu L, He D, Huang Q, Ke C, Li Z, Yu H, Klena JD, Wu S. Serotypes, seasonal trends, and antibiotic resistance of non-typhoidal Salmonella from human patients in Guangdong Province, China, 2009–2012. BMC Infect Dis. 2015;15:53.
Todd ECD. Foodborne disease and food control in the Gulf States. Food Control. 2017;73:341–66.
Wu G, Wang L, Wang Q, et al. Descriptive Study of Foodborne Disease Using Case Monitoring Data in Shandong Province, China, 2016–2017. Iran J Public Health. 2019;48(4):722–9.
Dewey-Mattia D, Manikonda K, Hall AJ, Wise ME, Crowe SJ. Surveillance for Foodborne Disease Outbreaks - United States, 2009–2015. MMWR Surveill Summ. 2018;67(10):1–11.
Kim JJ, Ryu S, Lee H. Foodborne Illness Outbreaks in Gyeonggi Province, Korea, Following Seafood Consumption Potentially Caused by Kudoa septempunctata between 2015 and 2016. Osong Public Health Res Perspect. 2018;9(2):66–72.
Wu YN, Liu XM, Chen Q, et al. Surveillance for foodborne disease outbreaks in China, 2003 to 2008. Food Control. 2018;84:382–8.
Schlinkmann KM, Razum O, Werber D. Characteristics of foodborne outbreaks in which use of analytical epidemiological studies contributed to identification of suspected vehicles, European Union, 2007 to 2011. Epidemiol Infect. 2017;145(6):1231–8.
Qi XL, Wang HX, Bu SR, Xu XG, Wu XY, Lin DF. Incidence rates and clinical Symptoms of Salmonella, Vibrio parahaemolyticus, and Shigella infections in China, 1998–2013. J Infect Dev Ctries. 2016;10(2):127–33.
Acknowledgements
The authors thank the food safety staff of the CDC at all levels of the province for their positive role and responsible handling of foodborne cases and timely submitting accurate reports, which enabled current study to have a large number of data to analyze the epidemiological characteristics of which in our province and put forward targeted intervention measures for further prevention and control.
Funding
This research was sponsored by Medical and Health Science and Technology Project of Zhejiang Province (No.2022KY712), Chinese National Natural Science Foundation (81973055), the National Key Research and Development Programme of China (No.2021YFC2701901), Major research and development projects of the Zhejiang Science and Technology Department (2018C03010), Key Laboratory of Intelligent Preventive Medicine of Zhejiang Province (2020E10004), and Leading Innovative and Entrepreneur Team Introduction Program of Zhejiang (2019R01007).
Author information
Authors and Affiliations
Contributions
X.J.Q. and X.A. made substantial contributions to the design of the work. X.J.Q. and X.A. drafted the work, Y.X.Y. and R.H.Z. substantively revised it. All authors made substantial contributions to the acquisition, analysis, and interpretation of data. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Zhejiang Provincial Center for Disease Control and Prevention (CDC). The study protocol was performed in accordance with the relevant guidelines. The ethics committee approved the procedure for verbal consent because Zhejiang CDC has the authority of the Zhejiang provincial government to collect and utilize information on foodborne disease cases, which is part of disease surveillance scope in Zhejiang CDC. All participants were informed that they had the right to reject or terminate the study at any time during the interview. Since we have obtained verbal consent, documentation of consent was not required. The information provided by each participant is confidential in Zhejiang CDC. The China’s National Center for Food Safety Risk Assessment (CFSA) is responsible for maintaining and managing the foodborne disease case surveillance system, and our use of the data has been verbally approved by CFSA.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiaojuan Qi and Xialidan Alifu contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qi, X., Alifu, X., Chen, J. et al. Descriptive study of foodborne disease using disease monitoring data in Zhejiang Province, China, 2016–2020. BMC Public Health 22, 1831 (2022). https://doi.org/10.1186/s12889-022-14226-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-14226-1