- Research
- Open access
- Published:
Prevalence and predictors of water-borne diseases among elderly people in India: evidence from Longitudinal Ageing Study in India, 2017–18
BMC Public Health volume 22, Article number: 993 (2022)
Abstract
Background
India suffers from a high burden of diarrhoea and other water-borne diseases due to unsafe water, inadequate sanitation and poor hygiene practices among human population. With age the immune system becomes complex and antibody alone does not determine susceptibility to diseases which increases the chances of waterborne disease among elderly population. Therefore the study examines the prevalence and predictors of water-borne diseases among elderly in India.
Method
Data for this study was collected from the Longitudinal Ageing Study in India (LASI), 2017–18. Descriptive statistics along with bivariate analysis was used in the present study to reveal the initial results. Proportion test was applied to check the significance level of prevalence of water borne diseases between urban and rural place of residence. Additionally, binary logistic regression analysis was used to estimate the association between the outcome variable (water borne diseases) and the explanatory variables.
Results
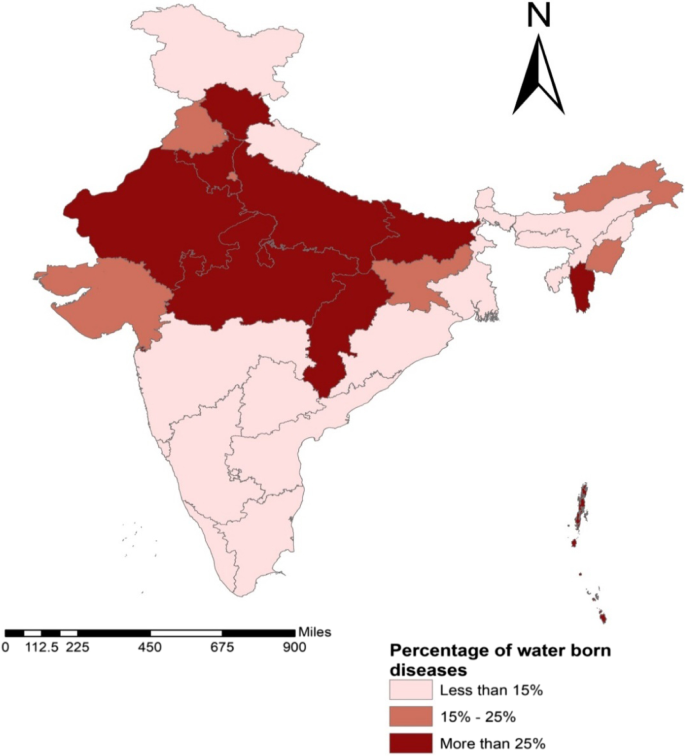
The study finds the prevalence of water borne disease among the elderly is more in the rural (22.5%) areas compared to the urban counterparts (12.2%) due to the use of unimproved water sources. The percentage of population aged 60 years and above with waterborne disease is more in the central Indian states like Chhattisgarh and Madhya Pradesh followed by the North Indian states. Sex of the participate, educational status, work status, BMI, place of residence, type of toilet facility and water source are important determinants of water borne disease among elderly in India.
Conclusion
Elderly people living in the rural areas are more prone to waterborne diseases. The study also finds state wise variation in prevalence of waterborne diseases. The elderly people might not be aware of the hygiene practices which further adhere to the disease risk. Therefore, there is a need to create awareness on basic hygiene among this population for preventing such bacterial diseases.
Introduction
The Sustainable Development Goal, 2017 aimed to ensure availability and sustainable management of water and sanitation for all by 2030 [1]. However globally 780 million people live without access to safe water and approximately 2.5 billion people in the developing world lived without access to adequate sanitation [2, 3]. Polluted water and poor sanitation practices expose individuals to health risks. Emerging water-borne pathogens constitute a significant health hazard in both developed and developing nations [4] as they can spread rapidly and affect large sections of the population. Water-borne diseases are transmitted through contaminated drinking water with pathogen microorganisms such as protozoa, virus, bacteria, and intestinal parasites. According to the projection of Global Burden Disease report, the burden of water borne disease was the second highest reason for mortality in 1990 however, it was lower down in ninth most important reason for mortality in 2020 [5]. Around 829,000 people are estimated to die each year from diarrheal diseases majorly cholera, dysentery and typhoid fever due to unsafe drinking water and unhygienic sanitation practice [6]. Further, the WHO (2015) reported that about 6.3 per cent of deaths occur due to unsafe water, inadequate sanitation, and poor hygiene. Adequate, safe, and accessible water supplies as well as satisfactory sanitation are most required to have secure health status [7]. According to WHO (2015), nearly 4 percent of the global disease burden could be prevented by improving water supply, sanitation, and hygiene [8].
It is estimated that around 37.7 million Indians are affected by waterborne diseases annually; 1.5 million children are estimated to die of diarrhoea alone and 73 million working days are lost due to waterborne disease each year [9]. Water-borne diseases pose a high disease burden and significantly impact on country’s economic growth [10]. These diseases erupt every year during summer and rainy seasons as a result of improper management of water supply especially of drinking water and sanitation [11, 12].
Poor urban governance, rapidly growing economies, highly dense population, poor housing and sanitation in slum areas of cities create environments rife for waterborne diseases [13]. One of the study in slum areas of Mumbai revealed that at least 30 per cent of all morbidity are due to water-related infections [14]. In rural areas, there are no proper water supply and sewerage systems. In the villages, water contamination can be attributed to infiltration, leaching, and surface run-off through pastures, lacking and leakage of sewerage disposal systems. Studies based on rural India revealed that lacking in knowledge, attitudes and practices (KAP) with regard to water handling, sanitation and defecation practices are common causes of waterborne diseases [15, 16]. Water pollution, open defecation and poor hygiene practices are the main hindrances to achieving good health. Therefore, safe and readily available water is essential for public health whether used for drinking, domestic use, food production or recreational purposes. Adequate access to safe water, improving quality of water source, treating and storing household water and encouraging hygiene practices can prevent waterborne diseases. As the global population is increasing rapidly over time, water availability will lower down steadily [8]. Individuals with low immunity are more susceptible to water-borne diarrheal diseases, especially children andelderly, with the low immune system are most susceptible to pathogen-related water-borne diseases [17]. According to U.S. Environmental Protection Agency, elderly along with children and pregnant women, were recognized as the sensitive sub-populations for water-borne diseases [18].
India is currently in the third stage of demographic transition and with 8% of geriatric population India could well be called an ageing nation [19]. The elderly population of India is expected to increase three fold by 2050 [20]. Among the elderly, infections are often more severe due to the presence of multiple underlying medical conditions, low immune system, and frequent use of drugs [21]. People in India mostly are unaware of safe and hygienic practices and this is prevalent across all age groups. This in turn increases the risk of communicable diseases. Thus, the resources and policy attention should be focused on strengthening primary health care systems that address communicable diseases and reduce the underlying risk factors. The rising number of elderly with various health problems creates a pressure on the existing public health system in India. In order to focus on strengthening the health care system to serve the elderly population there is need to study the prevalence of various disease risk among the elderly population. The major objective of the study is to examine the prevalence and predictors of water borne diseases among elderly. The study aims to bridge the research gap as less attention has been paid on the water borne diseases among the elderly population. The results of the study would further help in embarking knowledge, attitude and practices related to water handling, sanitation and defecation practices among the elderly which might reduce to some extent the load of communicable disease risk among elderly.
Materials and methods
Data
Study settings and population
Cross-sectional data for this study was used from the Longitudinal Ageing Study in India (LASI), nationally representative survey conducted in the year 2017–18 and covered 72,000 elderly age 45 and above across all states and union territories of India [22].
Study design
Cross-sectional survey.
Sample size calculation and sampling procedure
LASI is a full-scale national survey of scientific investigation of the health, economic, and social determinants and consequences of population aging in India. The main objective of the LASI survey was to study the health status and the social and economic well-being of elderly in India. The survey adopted a multistage stratified area probability cluster sampling design to arrive at the eventual units of observation: elderly age 45 and above and their spouses irrespective of age.
Within each state, LASI Wave 1 adopted three-stage sampling design in rural areas and four-stage sampling design in urban areas. In each state/UTs, the first stage involved selection of Primary Sampling Units (PSUs), that is, sub-districts (Tehsils/Talukas), and the second stage involved the selection of villages in rural areas and wards in urban areas in the selected PSUs. In rural areas, households were selected from selected villages in the third stage. However, sampling in urban areas involved an additional stage. Specifically, in the third stage, one Census Enumeration Block (CEB) was randomly selected in each in urban area. In the fourth stage, households were selected from this CEB.
The present study is conducted on the eligible participant’s age 60 years and above. The total sample size for the present study is 31464 (for rural-20725 and urban-10739) elders aged 60 years and above [22].
Study variables
Outcome variable
The outcome variable (water borne diseases) was binary in nature i.e. water borne diseases coded as no and yes. The variable was generated using the question “has any health professional diagnosed you with diarrhoea/gastroenteritis or typhoid or jaundice/hepatitis in last two years [23].
Explanatory variables
The control variables were selected after doing extensive literature review. The variables selected are as follows:
-
1.
Age was recoded as 60–69, 70–79 and 80 + years.
-
2.
Sex was recoded as male and female.
-
3.
Education was recoded as no education/primary not completed, primary completed, secondary completed and higher and above.
-
4.
Marital status was recoded as currently married, widowed and others. Others included separated/never married/divorced.
-
5.
Working status was coded as currently working, retire and never worked.
-
6.
Body mass index was recoded as underweight, normal and overweight/obese. The participants having a body mass index (BMI) of 25 and above were categorized as obese/overweight whereas participant who had BMI as 18.4 and less were coded as underweight [24]. BMI is calculated by dividing an individual’s weight (in kilograms) by the square of their height (in metres).
-
7.
Type of toilet facility was recoded as unimproved and improved [25]. Improved toilet facility includes pour-flush latrines, ventilated improved pit latrines, and pit latrines with a slab/covered pit. Unimproved toilet facility includes Shared facilities of any type, no facilities (bush or field); flush or pour-flush to elsewhere (that is, not to piped sewer system, septic tank or pit latrine); pit latrines without slab / open pits, bucket systems; hanging toilet or hanging latrine.
-
8.
Source of drinking water was recoded as unimproved and improved [25]. Improved source of drinking water includes piped water, public tap/standpipe, tube well or bore well, dug well, spring water and rain water. Unimproved water sources include tanker, cart with small tank, bottled water/pouch water, surface water and other sources of water.
-
9.
Type of house was recoded as pucca, semi pucca and kutcha.
-
10.
The monthly per capita expenditure (MPCE) was assessed using household consumption data. Sets of 11 and 29 questions on the expenditures on food and non-food items, respectively, were used to canvas the sample households. Food expenditure was collected based on a reference period of seven days, and non-food expenditure was collected based on reference periods of 30 days and 365 days. Food and non-food expenditures have been standardized to the 30-day reference period. The monthly per capita consumption expenditure (MPCE) is computed and used as the summary measure of consumption. The variable was then divided into five quintiles i.e., from poorest to richest [22].
-
11.
Religion was recoded as Hindu, Muslim, Christian and Others.
-
12.
Caste was recoded as Scheduled Tribe, Scheduled Caste, Other Backward Class, and others. The Scheduled Caste include “untouchables”; a group of the population that is socially segregated and financially/economically by their low status as per Hindu caste hierarchy. The Scheduled Castes (SCs) and Scheduled Tribes (STs) are among the most disadvantaged socio-economic groups in India. The OBC is the group of people who were identified as “educationally, economically and socially backward”. The OBC’s are considered low in the traditional caste hierarchy but are not considered untouchables. The “other” caste category is identified as having higher social status [26].
-
13.
Place of residence was recoded as rural and urban area.
-
14.
Region was recoded as North, Central, East, Northeast, West, and South.
Statistical analysis
Univariate along with bivariate analysis was used in present study to reveal the initial results. Proportion test [27] was applied to check the significance level of prevalence of water borne diseases between urban and rural place of residence. Additionally, binary logistic regression analysis [28] was used to estimate the association between the outcome variable (water borne diseases) and other explanatory variables.
The binary logistic regression model is usually put into a more compact form as follows:
The parameter \({\beta }_{0}\) estimates the log odds of water borne diseases for the reference group, while \(\beta\) estimates the maximum likelihood, the differential log odds of water borne diseases associated with a set of predictors X, as compared to the reference group, and \(\epsilon\) represents the residual in the model. The variance inflation factor (VIF) ( Additional file -Table-A1) was used to check for the presence of multicollinearity and the test confirmed that there was no evidence of multicollinearity [29]. STATA 14 was used for the analysis purpose.
Results
Socio-demographic and economic profile of elderly in India
Table 1 presents the socio-demographic and economic profile of the study participants. A similar proportion of elderly lived in rural and urban areas irrespective of age group. Only three per cent of elderly in rural areas had higher education and this percentage was five times in urban areas. In rural areas, about one-third of elderly were working whereas one-fifth of elderly in urban areas were working. Nearly one-third of older adults in rural and one in every ten older elderly in urban areas were underweight. Only one-third of elderly in rural areas were used improved toilet facility and eight in every 10 elderly in urban areas were used improved toilet facility. In rural areas, three fifth of elderly used improved source of drinking water whereas nine in every ten elderly from urban areas used improved source of drinking water. About four in every ten elderly in rural areas lived in pucca house and this proportion was almost double in urban areas.
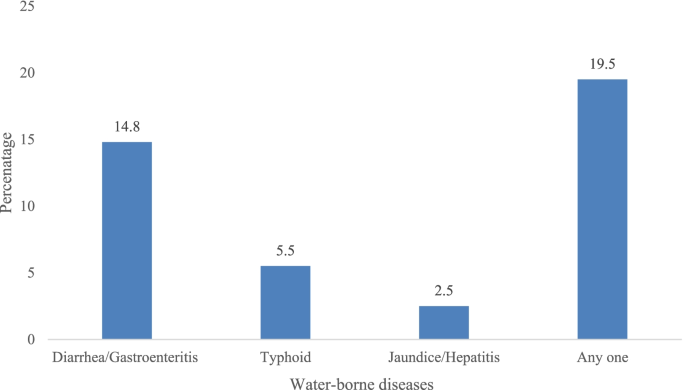
Figure 1 shows the prevalence of diarrhoea/gastroenteritis or typhoid or jaundice/hepatitis. It was found that 14.8% (14.4–15.2) of elderly suffered from diarrhoea/gastroenteritis and 5.5% (5.2–5.7) suffered from typhoid and 2.5% (2.3–2.7) suffered from jaundice/hepatitis. The prevalence of water borne diseases among elderly was 19.5% (19.0–19.8).
Prevalence of water borne diseases among elderly in India
Table 2 shows that there was a significant rural–urban difference in the prevalence of water borne diseases in India (difference: 10.2 percentage point). The prevalence of water borne disease among elderly in rural areas was 22.5% whereas in urban areas the prevalence was 12.2%. The rural–urban differences was highest among elderly who used unimproved toilet facility (difference: 17.1 percentage point), had 80 + years of age (difference: 14.4 percentage point), who belonged to other backward class (difference: 12.4 percentage point), richer elderly (difference: 12.3 percentage point), and those were not working (difference: 12.1 percentage point). Moreover, the prevalence of water borne diseases was higher among underweight elderly, and those who lived in kutcha houses irrespective to their place of residence.
Figure 2 shows state-wise prevalence of water borne diseases among elderly in India. The prevalence of water borne diseases was highest in Chhattisgarh (36.9 per cent), followed by Mizoram (35 per cent), Haryana (34.6 per cent), and Bihar (34 per cent). However, this prevalence was lowest in Kerala (3.5 per cent), followed by Goa (6.2 per cent), and Tamil Nadu (6.8 per cent).
State-wise prevalence of water borne diseases in rural and urban areas in India
Table 3 presents the state-wise prevalence of water borne disease stratified by place of residence in India. In rural areas, the prevalence of water borne diseases was highest in Chhattisgarh (38.5 per cent) followed by Madhya Pradesh (36 per cent), Haryana (35.2 per cent), and Rajasthan (34.9 per cent) while for urban areas, water borne diseases was more prevalent in Bihar (36.3 per cent), followed by Mizoram (36.1 per cent), Himachal Pradesh (32.9 per cent), and Haryana (32.4 per cent) [Additional file Table A2].
Estimates from logistic regression analysis for older adults who suffered from water borne diseases in India
Table 4 shows the adjusted odds ratio for elderly who suffered from water borne disease in India. It was revealed that the odds of water borne diseases was high in rural areas in reference to urban areas [AOR: 1.21; p < 0.05]. The likelihood of water borne diseases was significantly more among elderly female than male counterparts [AOR: 1.19; p < 0.05]. Moreover, the odds of water borne diseases were decreased with increase the level of education among elderly. The risk of water borne diseases was 12 per cent more among underweight elderly compared to overweight/obese elderly [AOR: 1.12; p < 0.05]. Similarly, elderly who used unimproved toilet facility [AOR: 1.22; p < 0.05] and unimproved source of drinking water [AOR: 1.37; p < 0.05] were 22 per cent and 37 per cent more likely to suffer from water borne diseases respectively, compared to their counterparts. The likelihood of water borne diseases was 27 per cent and 16 per cent more among scheduled tribe [AOR: 1.27; p < 0.05] and other backward class elderly [AOR: 1.16; p < 0.05] respectively, compared to scheduled caste elderly. With reference to elderly who belonged to North region, the likelihood of water borne diseases was 36 per cent more among elderly who belonged to Central region [AOR: 1.36; p < 0.05].
Discussion
The present study tries to see the prevalence and predictors of water borne disease in India. The prevalence of water borne disease among the elderly is more in the rural (22.5%) areas compared to the urban counterparts (12.2%) with a significant absolute difference of about 10.2%. The percentage of elderly population with waterborne disease is more in the central Indian states like Chhattisgarh and Madhya Pradesh followed by the North Indian states. The result of logistic regression concludes that sex of the participant, educational status, working status, BMI, place of residence, type of toilet facility and water source are important determinants of water borne disease among elderly in India. The infectious disease distribution which includes water borne diseases involves complex social and demographic factors including human population density and behaviour, housing type and location, water supply, sewage and waste management systems, land use and irrigation systems, access to health care, and general environmental hygiene [30]. In the study the waterborne diseases include diarrhoea, typhoid and jaundice. Earlier studies have shown diarrhoea and its complication to be more among elderly people, particularly those who require long term care [31]. The study finding that waterborne diseases are more in the rural areas compared to the urban areas is also consistent with earlier studies which concluded diarrheal prevalence to be more in rural areas and also in Central part of the country [32, 33]. A meta-analysis of typhoid prevalence in India concluded that this waterborne disease prevalence was more in the rural area with 0.09 lesser odds of having the disease in urban counterparts [34].
Our finding that waterborne disease prevalence vary with the anthropometric status as measured by BMI level with significantly higher odds of prevalence among the underweight compared to the overweight participants have theoretical justification as well. The relationship between malnutrition and the infection risk is bidirectional where infection adversely affects nutritional status through reductions in dietary intake and intestinal absorption, increased catabolism and sequestration of nutrients that are required for tissue synthesis and growth. On the other hand, malnutrition can predispose to infection because of its negative impact on the barrier protection afforded by the skin and mucous membranes and by inducing alterations in host immune function [35,36,37]. Earlier studies based on infectious disease risk among the children have indicated the educational status of mother as an important determinant with more infections among illiterate mothers [32, 38, 39]. The studies have debated that the disease risk is lesser among educated mothers because of hygiene practices, child feeding and caring practices, and improved living conditions. Similarly among the elderly participants as well educated people have a better understanding of the hygiene practices and feeding and caring habits and hence a reduced risk of waterborne infections.
The study finding that disease risk is more among population using unimproved sources of water and sanitation is consistent with earlier study which states drinking water, sanitation facilities and hygienic behaviour are the determining factors of health of household members [40]. A longitudinal study in the slums of Ethiopia shows sanitation facilities and hygienic condition of households were associated with acute diarrhoea [41]. Studies have also indicated improved water, sanitation and hygiene conditions of the households are accountable for diarrheal and other waterborne diseases [42, 43]. Unimproved sources of drinking water, quality of drinking water, absences of sanitation facilities and garbage collection was associated with stomach problem in urban India [16, 44, 45].
India suffers from a higher burden of infectious disease particularly water bone disease due to a weak public drinking water distribution system [10]. The degraded water quality can contribute to water scarcity as it limits its availability for both human use and for the ecosystem. With more than 8% of elderly aged 60 years and above residing in India [19] it is important to see the prevalence of water borne disease among the increasing population of elderly as there is a need to protect the population since treatment cost is also not cheap. Moreover, studies indicating infectious disease among the elderly is very few [21]. Thus the present analysis is an important contribution in research related to health of the elder population.
Conclusion
Elderly living in rural areas are more prone to waterborne diseases. Use of unimproved water and absence of improved sanitation are major factors affecting waterborne disease among elderly. However the major limitation of the study is that the disease prevalence is based on self-reported morbidity status and lacks clinical verification, with a possibility of under reporting as well as over reporting and thus an underestimation or overestimation of the prevalence of the morbidities under study. However as is seen in various studies these self-reported measures or patient reported outcomes address issues that are of primary interest to the clinician and thus can be considered for measurement [23]. Consistent with findings from earlier literature regardless of whether there is under-reporting or over-reporting, the aforesaid socio-economic and demographic factors affect the pattern of morbidities associated with infections among elderly in India.
The elderly population might not be aware of the hygiene practices which adhere to the disease risk among this group. With age the antibody resistance falls and thus they might be well affected by the waterborne diseases. There is a need to focus on this population on preventing such bacterial diseases. This can be achieved by encouraging those aged 60 years and above as well as their caretakers to seek healthcare at early signs of infection. It also recommends making elderly aware of how to maintain the proper hygienic condition while availing the improved sanitation and water facilities provided to the people. The government should focus on providing safe water to the elderly population, train them to store water in a right and proper way.
Availability of data and materials
References
United Nations. The Millennium Development Goals Report. United Nations 2015:72. 978-92-1-101320-7
Agingu JB. Levels and differentials of occurence of water borne diseases at Moi University. Kenya Acad Res Int. 2020;11:10–8.
Bidhuri S, Taqi M, Khan MMA. Water-borne disease: Link between human health and water use in the Mithepur and Jaitpur area of the NCT of Delhi. J Public Heal. 2018;26:119–26. https://doi.org/10.1007/s10389-017-0835-y.
Sharma S, Sachdeva P, Virdi JS. Emerging water-borne pathogens. Appl Microbiol Biotechnol. 2003;61(5-6):424-8. https://doi.org/10.1007/s00253-003-1302-y. Epub 2003 Apr 9.
Lopez AD, Murray CJ, eds., The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020; summary. Harvard School of Public Health; 1996.
Prüss-Ustün A, Bartram J, Clasen T, Colford JM Jr, Cumming O, Curtis V, et al. Burden of disease from inadequate water, sanitation and hygiene in low-and middle-income settings: a retrospective analysis of data from 145 countries. Trop Med Int Heal. 2014;19:894–905.
Szálkai K. Water-Borne Diseases BT - The Palgrave Encyclopedia of Global Security Studies. In: Romaniuk S, Thapa M, Marton P, editors. Cham: Springer International Publishing; 2019. pp. 1–7. https://doi.org/10.1007/978-3-319-74336-3_562-1.
WHO/UNICEF Joint Water Supply, & Sanitation Monitoring Programme. Progress on sanitation and drinking water: 2015 update and MDG assessment. World Health Organization; 2015.
UNICEF. Clean drinking water Ensuring survival and improved outcomes across all outcomes for every child. 2019.
Pathak H. Effect of Water Borne Diseases on Indian Economy…. Analele Univ Din Ordea, Ser Geogr. 2015;1:74–8.
Chabba APS. Water-Borne Diseases in India. 2013.
Oguntoke O, Aboderin OJ, Bankole AM. Association of water-borne diseases morbidity pattern and water quality in parts of Ibadan City. Nigeria. 2009;11:189–95.
Saravanan VS, Ayessa Idenal M, Saiyed S, Saxena D, Gerke S. Urbanization and human health in urban India: Institutional analysis of water-borne diseases in Ahmedabad. Health Policy Plan. 2016;31:1089–99. https://doi.org/10.1093/heapol/czw039.
Karn SK, Harada H. Field survey on water supply, sanitation and associated health impacts in urban poor communities – a case from Mumbai City, India. Water Science and Technology. 2002;46(11-12):269-75.
Banda K, Sarkar R, Gopal S, Govindarajan J, Harijan BB, Jeyakumar MB, et al. Water handling, sanitation and defecation practices in rural southern India: a knowledge, attitudes and practices study. Trans R Soc Trop Med Hyg. 2007;101:1124–30. https://doi.org/10.1016/j.trstmh.2007.05.004.
Purohit BC. Health Impact of Water Borne Diseases and Regional Disparities in India. Int J Heal Sci Res Int J Heal Sci Res. 2012;2:1.
Pal M, Ayele Y, Hadush A, Panigrahi S, Jadhav VJ. Public Health Hazards Due to Unsafe Drinking Water. Air Water Borne Dis. 2018;7:1–6. https://doi.org/10.4172/2167-7719.1000138.
Naumova EN, Egorov AI, Morris RD, Griffiths JK. The elderly and waterborne Cryptosporidium infection: Gastroenteritis hospitalizations before and during the 1993 Milwaukee outbreak. Emerg Infect Dis. 2003;9:418–25. https://doi.org/10.3201/eid0904.020260.
Office of the Registrar General & Census Commissioner of India. Census of India 2011 provisional population totals. Ministry of Home Affairs, Government of India. 2011.
Bhagat RB. "Ageing in India: The Class Demographics and Policy Issues." The Trajectory of India’s Middle Class. Economy, Ethics and Etiquette. 2015:248-263.
Steens A, Eriksen HM, Blystad H. What are the most important infectious diseases among those ≥65 years: a comprehensive analysis on notifiable diseases, Norway, 1993-2011. BMC Infect Dis. 2014;14:57. https://doi.org/10.1186/1471-2334-14-57.
International Institute for Population Sciences (IIPS), NPHCE, MoHFW, et al. Longitudinal Ageing Study in India (LASI) Wave 1. Mumbai, India (2020).
McKenna SP. Measuring patient-reported outcomes: Moving beyond misplaced common sense to hard science. BMC Med. 2011;9:86. https://doi.org/10.1186/1741-7015-9-86.
Fauziana R, Jeyagurunathan A, Abdin E, Vaingankar J, Sagayadevan V, Shafie S, et al. Body mass index, waist-hip ratio and risk of chronic medical condition in the elderly population: Results from the Well-being of the Singapore Elderly (WiSE) Study. BMC Geriatr. 2016;16:1–9. https://doi.org/10.1186/s12877-016-0297-z.
Kumar P, Patel R, Chauhan S, Srivastava S, Khare A, Kumar PK. Does socio-economic inequality in infant mortality still exists in India? An analysis based on National Family Health Survey 2005–06 and 2015–16. Clin Epidemiol Glob Heal. 2020. https://doi.org/10.1016/j.cegh.2020.07.010.
Zacharias A, Vakulabharanam V. Caste Stratification and Wealth Inequality in India. World Dev. 2011. https://doi.org/10.1016/j.worlddev.2011.04.026.
Koopman PAR. Confidence Intervals for the Ratio of Two Binomial Proportions. Biometrics. 1984. https://doi.org/10.2307/2531405.
King J. Binary logistic regression. In Osborne, J. (Ed.), Best practices in quantitative methods (pp. 358-384). SAGE Publications, Inc.; 2008. https://dx.doi.org/10.4135/9781412995627.
Lewis-Beck M, Bryman A, Futing LT. Variance Inflation Factors. SAGE Encycl Soc Sci Res Methods. 2012. https://doi.org/10.4135/9781412950589.n1067.
Ramana Dhara V, Schramm PJ, Luber G. Climate change & infectious diseases in India: Implications for health care providers. Indian J Med Res. 2013;138:847–52.
Adiga GU, Dharmarajan TS, Pitchumoni CS. Diarrhea in older adults. Pract Gastroenterol. 2005;29:63–82.
Paul P. Socio-demographic and environmental factors associated with diarrhoeal disease among children under five in India. BMC Public Health. 2020;20:1–11. https://doi.org/10.1186/s12889-020-09981-y.
Vijayan B, Ramanathan M. Prevalence and clustering of diarrhoea within households in India: some evidence from NFHS-4, 2015–16. J Biosoc Sci. 2013;53:108–20. https://doi.org/10.1017/s0021932020000073.
John J, Van Aart CJC, Grassly NC. The Burden of Typhoid and Paratyphoid in India: Systematic Review and Meta-analysis. PLoS Negl Trop Dis. 2016;10:1–14. https://doi.org/10.1371/journal.pntd.0004616.
Martorell R, Habicht JP, Yarbrough C, Lechtig A, Klein RE, Western KA. Acute morbidity and physical growth in rural Guatemalan children. Am J Dis Child. 1975;129:1296–301. https://doi.org/10.1001/archpedi.1975.02120480022007.
Palmer DL, Koster FT, Alam AKMJ, Islam MR. Nutritional Status: A Determinant of Severity of Diarrhea in Patients with Cholera. J Infect Dis. 1976;134:8–14. https://doi.org/10.1093/infdis/134.1.8.
Kenneth BH. Symposium: Nutrition and Infection, Prologue and Progress Since 1968: Diarrhea and Malnutrition. J Nutr. 2003;133:336–40.
Sarker AR, Sultana M, Mahumud RA, Sheikh N, Van Der Meer R, Morton A. Prevalence and Health Care-Seeking Behavior for Childhood Diarrheal Disease in Bangladesh. Glob Pediatr Health. 2016;3:2333794X16680901. https://doi.org/10.1177/2333794X16680901.
Asfaha KF, Tesfamichael FA, Fisseha GK, Misgina KH, Weldu MG, Welehaweria NB, Gebregiorgis YS. Determinants of childhood diarrhea in Medebay Zana District, Northwest Tigray, Ethiopia: a community based unmatched case-control study. BMC Pediatr. 2018;18(1):120. https://doi.org/10.1186/s12887-018-1098-7.
Troeger C, Forouzanfar M, Rao PC, Khalil I, Brown A, Reiner RC, et al. Estimates of global, regional, and national morbidity, mortality, and aetiologies of diarrhoeal diseases: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect Dis. 2017;17:909–48. https://doi.org/10.1016/S1473-3099(17)30276-1.
Adane M, Mengistie B, Kloos H, Medhin G, Mulat W. Sanitation facilities, hygienic conditions, and prevalence of acute diarrhea among underfive children in slums of Addis Ababa, Ethiopia: Baseline survey of a longitudinal study. PLoS ONE. 2017;12:1–18. https://doi.org/10.1371/journal.pone.0182783.
Bakir H, Hadi M, Jurdi M. Towards a renewed public health regulatory and surveillance role in water, sanitation and hygiene. East Mediterr Health J. 2017;23(8):525-6.
Fan VYM, Mahal A. What prevents child diarrhoea? the impacts of water supply, toilets, and hand-washing in rural India. J Dev Eff. 2011;3:340–70. https://doi.org/10.1080/19439342.2011.596941.
Kumar S, Vollmer S. Does access to improved sanitation reduce childhood diarrhea in rural India? Health Econ. 2013;22(4):410-27. https://doi.org/10.1002/hec.2809. Epub 2012 Mar 22.
Patel SK., Pradhan MR, Patel S. Water, sanitation, and hygiene (WASH) conditions and their association with selected diseases in urban India. J Popul and Soc Stud [JPSS]. 2020;28(2):103-15.
Acknowledgements
Not applicable.
Accordance statement
This study is not based any experiments on humans data.
Funding
No.
Author information
Authors and Affiliations
Contributions
Conception and design of study: PK, and SS; analysis and interpretation of data: PK and SS; drafting the manuscript: PK, SS, AB, SB; All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The data is freely available on request and survey agencies that conducted the field survey for the data collection have collected a prior consent from the respondent. The ethical clearance was provided by Indian Council of Medical Research (ICMR), India.
Consent for publication
Not applicable.
Competing interests
No.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kumar, P., Srivastava, S., Banerjee, A. et al. Prevalence and predictors of water-borne diseases among elderly people in India: evidence from Longitudinal Ageing Study in India, 2017–18. BMC Public Health 22, 993 (2022). https://doi.org/10.1186/s12889-022-13376-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-13376-6