- Research
- Open access
- Published:
Infectious disease surveillance for refugees at borders and in destination countries: a scoping review
BMC Public Health volume 22, Article number: 227 (2022)
Abstract
Background
Data on infectious disease surveillance for migrants on arrival and in destination countries are limited, despite global migration increases, and more are needed to inform national surveillance policies. Our study aimed to examine the scope of existing literature including existing infectious disease surveillance activities, surveillance methods used, surveillance policies or protocols, and potential lessons reported.
Methods
Using Arksey and O’Malley’s six-stage approach, we screened four scientific databases systematically and 11 websites, Google, and Google Scholar purposively using search terms related to ‘refugee’ and ‘infectious disease surveillance’ with no restrictions on time-period or country. Title/abstracts and full texts were screened against eligibility criteria and extracted data were synthesised thematically.
Results
We included 20 eligible sources of 728 identified. Reporting countries were primarily European and all were published between 1999 and 2019. Surveillance methods included 9 sources on syndromic surveillance, 2 on Early Warning and Response (EWAR), 1 on cross-border surveillance, and 1 on GeoSentinel clinic surveillance. Only 7 sources mentioned existing surveillance protocols and communication with reporting sites, while policies around surveillance were almost non-existent. Eleven included achievements such as improved partner collaboration, while 6 reported the lack of systematic approaches to surveillance.
Conclusion
This study identified minimal literature on infectious disease surveillance for migrants in transit and destination countries. We found significant gaps geographically and on surveillance policies and protocols. Countries receiving refugees could document and share disease surveillance methods and findings to fill these gaps and support other countries in improving disease surveillance.
Background
Disease surveillance contributes to epidemic control and other important public health responses [1,2,3]. The World Health Organization (WHO) defines disease surveillance as “ongoing systematic collection, analysis, and interpretation of outcome-specific data for use in planning, implementing and evaluating public health policies and practices” [4]. Surveillance differs from medical screening, the aim of which is clinical, as surveillance is broader and involves analysing health issues for disease interventions and prevention [4,5,6]. Infectious disease surveillance provides ongoing information on the health status of a population, which contributes to morbidity and mortality prevention, improves health service provision, and guides population health programmes [4, 7, 8].
Surveying and quantifying the healthcare needs of displaced populations, especially newly arrived ones, is important for disease prevention and resource allocation for often vulnerable people [9, 10]. Infectious disease surveillance during humanitarian crises can enable ongoing information for action, especially in displacement settlements [4, 7, 8]. Both formal (e.g. traditional ‘refugee camps’) and informal displacement settlements can be overcrowded and lack basic needs, e.g. water, sanitary supplies, nutritious food, and environmental protection [4, 7, 8]. Infectious disease concerns among refugees arriving in destination countries are diverse, with a recent review among asylum-seekers and refugees in Europe for 2010–2016 finding tuberculosis and Hepatitis B most prevalent with malaria, Hepatitis C, cutaneous diphtheria, louse-born relapsing fever, and shigellosis also common [11]. The United Nations Refugee Agency (UNHCR) reported that 75% of outbreaks in its refugee camps in 2009–2017 were due to measles, cholera, and meningitis [12]. Hence, disease surveillance is required for identifying outbreaks and initiating timely interventions.
From 2011, Europe experienced significantly increased forced migration from Syria along with other war-devastated countries in the Eastern Mediterranean, South Asia, and North Africa regions [13,14,15]. Consequently, the European Centres for Disease Control (ECDC) encouraged establishment of syndromic surveillance for refugee populations within routine national surveillance systems [13, 14]. Syndromic surveillance entails early detection of possible disease outbreaks by using clinical rather than laboratory confirmed diagnoses to enable faster responses that can reduce morbidity and mortality [14, 16]. In 2016, ECDC published a three-phase guidance (i.e. preparatory, pilot, implementation) on establishing syndromic surveillance systems for countries receiving refugees [13, 14]. This helped countries such as Germany, Greece, Italy, and Spain, develop syndromic surveillance to respond more quickly to migrants taking the Mediterranean route [15, 17,18,19,20,21].
We aimed to identify and summarize the literature related to infectious diseases surveillance targeting refugees at borders or in destination countries. Objectives were to: (i) identify national, international, and cross-border infectious diseases surveillance activities targeting refugees; (ii) examine how these surveillance activities were conducted, including protocols, regulations, and policies developed in relation to surveillance activities; and (iii) synthesise any major achievements or challenges identified.
Methods
Study design
We conducted a scoping review, using Arksey and O’Malley’s six-stage framework with Levac et al’s revisions, as detailed in Woodward et al. [22]. These stages are: (i) defining the research question; (ii) identifying documentary sources addressing the research question; (iii) selecting sources that meet inclusion criteria; (iv) charting/extracting relevant data; (v) synthesising and analysing data; and (iv) consulting topic experts to identify additional sources or sense-check initial findings as appropriate. We selected a scoping design anticipating that our literature would be limited to relatively few sources and heterogeneous in design, type, methods, focus, and quality.
Defining the research question
Our research question was: “What is the scope and nature of the literature on infectious disease surveillance for refugees, as defined either by mandate or 1951 Convention, including surveillance methods, policies/protocols, and lessons learned?”
Identifying sources
The lead author searched four databases systematically (i.e. EMBASE, Global Health, PubMed, Jstor), 11 selected websites purposively (i.e. International Organization for Migration [IOM], Eurosurveillance, World Health Organization [WHO], including six regional office sites, bulletins, weekly epidemiological record), and Google and Google Scholar purposively for the first 100 hits. Purposive searching, as used for websites and search engines, is equivalent to non-probability sampling in that researchers rely on personal judgment to rapidly prioritise sources from a broad range of settings that are as relevant as possible to the review and contain sufficiently rich data [23].
Table 1 shows study definitions used. The search strategy used terms related to” refugee” and” infectious disease surveillance” [24, 26]. Our study focused on surveillance as opposed to screening [6], as the aim of the latter is primarily clinical and involves detecting specific diseases within a high-risk population not yet symptomatic [5, 6]. Screening is a short-term activity performed at different intervals, while surveillance is broader, continuous, and involves analysing health issues for disease interventions and prevention [4,5,6]. However, we included screening in our search terms, as they are sometimes used interchangeably, and manually excluded documents only addressing screening. Similarly, though our study focused on mandated refugees, we included terms related to ‘migrant,’ ‘displaced,’ and ‘asylum-seeker’ populations, so as not to miss relevant documents that used different terms for people we defined as refugees, and manually excluded ineligible documents. Search terms were consistent, with subheading and MESH terms revised as needed. For example, in Ovid EMBASE the search used: (disease surveillance OR screening [subheadings]) AND (migrant OR refugee OR “asylum seeker” OR “displaced” [search terms]) AND (syndromic OR infectious OR infection OR “communicable disease” [subheading]) AND (policy OR “organizational policy” OR “public policy” [subheadings] OR protocol [search term]).
Selecting sources
We agreed on eligibility criteria iteratively, from initial criteria based on the research question and research data sources (Table 2). The lead author removed duplicates using EndNote software and screened titles and abstracts, then remaining full texts, against eligibility criteria in discussion with co-authors. Issues were resolved by co-author consensus.
Extracting data
We extracted data from each source to an Excel file under the following headings: lead author, publication year, target population, study methods, surveillance system description, surveillance methods used, protocols and policies used, and lessons learned.
Synthesis
We collated descriptive data on included sources quantitatively (i.e. publication year, source type, countries included, primary methods, target populations described). We synthesised outcome data thematically on surveillance systems, methods, protocols/policies, and lessons learned, using a deductive approach described by Braun et al. [27].
Consulting stakeholders
The lead author presented initial findings at the XII International Epidemiological Association-Eastern Mediterranean Region Scientific Meeting in Beirut in 2019. Ten experts on surveillance and refugee health provided feedback during the presentation or informally afterwards, which the lead author recorded using a notebook and used to strengthen this review.
Results
Scope and nature of documents
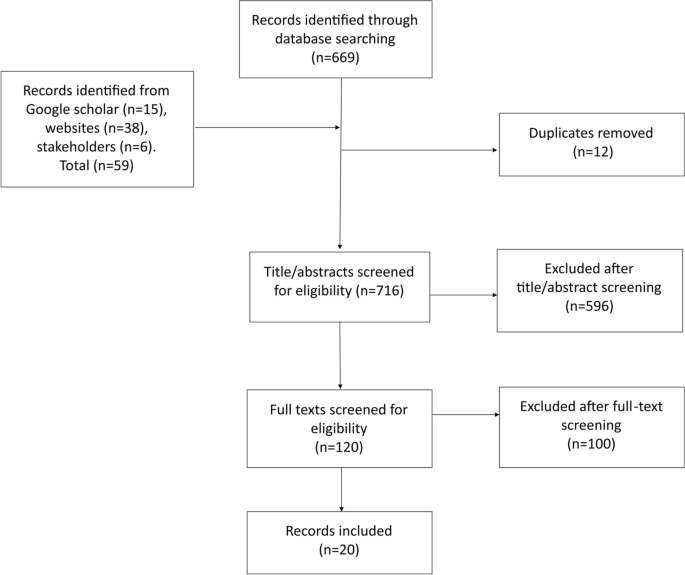
Figure 1 provides the PRISMA flow diagram for 20 sources included of 728 identified through searches. Publication dates began with one source in 1999 (5%) and increased somewhat to a peak of 4 in 2018 (21%), only one in 2019, and none in 2020. Twelve (60%) were journal articles, five (25%) were evaluation or technical reports, two (10%) were WHO updates on EWAR, and one (5%) was a letter to editors.
Countries included were diverse, but predominantly European (i.e. 13 sources), 4 for Italy, 2 for Greece, 1 each for Albania, Germany, Macedonia, and Spain, while 1 included six European countries, and 2 discussed Europe as a region [17,18,19,20,21, 28,29,30,31,32,33,34,35]. Three from the Africa region discussed camp-based surveillance in Cote d’Ivoire and Sudan, disputed Sudan-Chad borders, and Minawao in Cameroon [36,37,38]. Two from the Asia region discussed surveillance in Bangladesh and the Myanmar-Thailand border [39, 40]. One from the Americas region discussed binational surveillance on the United States (US)-Mexico border [41]. One source was global, including 24 countries [42].
Terminology was also diverse. Only 8 sources used the term ‘refugee’ in describing target populations [30, 33,34,35, 37,38,39,40], 8 used ‘migrant’ as a general term [15, 17, 19,20,21, 32, 41, 42], and 4 combined terms, describing ‘migrants and refugees’, ‘displaced and refugees’, ‘refugees and asylum-seekers’ as the population of interest [18, 28, 29, 36]. Most sources (13; 65%) were descriptive rather than analytical, while 4 conducted health system assessments [19,20,21, 37], 1 used scoping methods [28], 1 used descriptive epidemiological statistics [18], and 1 provided authors’ opinions [30].
Thematic synthesis
We synthesised outcomes under four deductive themes: (i) infectious disease surveillance targeting refugees and migrants; (ii) surveillance methods used; (iii) protocols and policies used; and (iv) reported lessons and limitations described. Table 3 summarises findings by source and theme.
Infectious disease surveillance targeting refugees and migrants
Most sources described migrant disease surveillance in Europe (13; 65%). In initial sources, published in 1999 and 2000, Valenciano et al and Brusin described syndromic disease surveillance systems established in two bordering countries, Albania and Macedonia, in response to the Kosovo crisis [34, 35].
After 2011, specific syndromic surveillance systems were developed in European countries to address increased migrant numbers more quickly. Three examples from Italy described disease surveillance for refugees, primarily from North Africa [15, 32, 33]. One described 6 months of syndromic surveillance in migration centres [32], results of 2 years of syndromic surveillance operated in parallel with existing routine statutory surveillance [15], and multiple other types of surveillance [33]. Riccardo et al. presented surveillance problems during migrant arrivals in the European Union (EU) in a letter to Eurosurveillance journal [30] and described the Common Approach for Refugees (CARE) Syndromic surveillance simulation implemented as a preparedness exercise in Italy [29].
WHO European Regional Office (EURO) assessed health system capacities of several migrant-receiving countries, including in Italy [19], Spain [20], and Greece [21]. The Italy assessment reported that Sicily had a syndromic surveillance system for migrants since 2011, while for the rest of Italy this appeared less active [19]. The Greece assessment suggested regular surveillance activities but no formal system established [21], while migrant disease surveillance was mentioned for Spain with no further details provided [20]. Syndromic surveillance systems were also documented in Greece [18] and Germany [17]. A scoping study, including key informant interviews in six European Union (EU) countries, described surveillance targeting refugees and asylum-seekers [28].
Two Asia region sources described a three-year enhanced hospital-based respiratory virus surveillance programme in a Myanmar refugee camp in Northwest Thailand, to examine pneumonia burden among migrants living on the border [40], and surveillance in Rohingya refugee camps in Cox’s Bazar Bangladesh (WHO-SEARO, 2018).
Two Africa region sources described Early Warning and Response (EWAR) networks in Darfur, Sudan, and Chad for displaced and refugee populations [36] and surveillance in Liberian refugee transit camps in Cote d’Ivoire [38]. One from Cameroon described activities of a diarrheal disease surveillance in Minawao refugee camp for an evaluation of the system [37].
One Americas region source described collaborative surveillance activities on the USA-Mexico border [41]. One global source briefly describes infectious disease surveillance activities in GeoSentinel clinic sites targeting migrants in 24 countries across six continents [42].
Surveillance methods
Five sources reported surveillance activities supervised or implemented by national public health institutes such as the Institute of Public Health in in Albania, the National Centre for Epidemiology and National Institute of Health in Italy, and Robert Koch Institute in Germany [15, 17, 20, 34, 35]. A few reported assistance or implementation of surveillance systems by international organizations such as WHO in Bangladesh, Darfur, Sudan and Chad, UNHCR and WHO in Macedonia, and US Centres for Disease Control (US-CDC) on the US-Mexico border [34,35,36, 39, 41].
Notifiable disease lists were mentioned for 7 countries, usually consisting of 12–14 diseases and syndromes that were similar across countries [17, 18, 32, 34,35,36]. For example, all lists included acute respiratory infections, meningitis, and diarrhoea. Others included nationally relevant diseases, such as malaria in Greece, Sudan, and Chad, or non-infectious concerns such as psychological and cardiovascular diseases in Albania [18, 34, 36]. Four mentioned the provision of case definitions along with the list [15, 17, 32, 34].
Reporting approaches were passive or active. For passive reporting, as documented in Albania, Macedonia, Italy, Germany, and Cote d’Ivoire transit camps, reports from camps or immigration centres were sent to reporting authorities via online database, fax, email, telephone, radio, or vehicle [15, 17, 34, 35, 38]. Active case finding, as documented in Albania, Cote d’Ivoire transit camps, Cameroon, and Thailand, included door-to-door searches and reviews of medical registers [34, 37, 38, 40]. Reporting speed was either immediate, if fitting immediate notifiable criteria as in Macedonia [35]; daily as in Italian, German, and Greek syndromic surveillance systems [17, 18, 32]; or weekly as in Albania and Cameroon [34, 37].
Coordination meetings between reporting authorities, surveillance teams, reporting sites, and stakeholders were conducted either daily as in Cote D’Ivoire transit camps, weekly as in Macedonia, or monthly as in Germany [17, 35, 38]. One source reported annual binational meetings for border surveillance between US and Mexico authorities [41]. Dissemination of information, as statistical reports or bulletins, was most often weekly and shared during coordination meetings, on national surveillance program websites, via email, or as hard copies [15, 17, 32, 34, 35, 38].
All except four sources described national surveillance systems that tracked migrants. Exceptions were subnational surveillance in Apulia Italy [33] and border areas of Myanmar [40]. Additionally, Waterman et al described binational cross-border surveillance collaboration, with common case definitions established [41]. Finally, McCarthy et al described global GeoSentinel surveillance, mainly through specialised travel and tropical medicine clinics [42].
Surveillance protocols, guidelines, and policies
Eight sources mentioned the existence of surveillance policies, protocols, or guidelines shared with reporting sites [15, 32, 33, 35, 37, 41,42,43]. Instead of a protocol document, Germany’s syndromic surveillance system team developed a toolkit hosted on an institutional website [17]. Some protocols were described as insufficient or poorly defined. For example, interviewees in several EU countries described their guidance on data collection and recording as inadequate [28]. Similarly, prior to the binational surveillance initiative, reporting protocols for US-Mexico land borders were described as poorly defined [41].
Policies related to surveillance were rarely mentioned. Only one source reported a surveillance-related policy change, in which the Italian surveillance system was extended beyond the humanitarian emergency end date to allow reporting centres to apply Italian infectious diseases statutory surveillance [15]. Conversely, Germinario et al. highlighted the EU’s need to enact infectious disease screening regulations for migrant populations [33]. A scoping study of six EU countries mentioned that “legal procedures” usually needed to be surpassed in destination countries, leading to ad-hoc activities [28].
Reported lessons and limitations
Nine sources reported that migrant-specific surveillance systems provided insight into infectious diagnoses and trends among refugees, enabled early detection of potential outbreaks, helped reduce disease transmission in camps, and led to obvious improvements in public health interventions [17, 32, 33, 36,37,38,39,40, 42].
Three reported the additional benefit of closer collaboration between partners or with refugee populations. For example, the Albania source reported that setting up the surveillance system led to close collaboration between surveillance team and health facilities, a task that would have been difficult outside the emergency context [34]. Kouadio et al recounted a reason behind their effective surveillance was cooperation between the surveillance team and refugee population [38]. Waterman et al emphasised cross-border coordination for achieving surveillance goals and common guidelines between US and Mexico [41].
Many sources described lessons on limitations that needed to be addressed. For example, two WHO assessments showed data collection was not systematic, with different databases maintained by different partners, and health-workers in migrant centres noting aspects of the syndromic surveillance system needed to be clarified [19, 21]. Similarly, another mentioned the lack of systematic approaches to surveillance, especially in the EU [30]. One noted that in Greece some diseases were identified through the mandatory notification system operating in parallel to the Points of Care surveillance system for refugees and migrants [18]. Another limitation mentioned was sustainability of surveillance for refugee populations. A study of six EU countries declared sustainability as almost impossible, resulting in ad-hoc systems [28]. Another source from Italy similarly highlighted that ad hoc surveillance cannot be sustained so needs to be corrected “before it can become a routine tool” [15].
Napoli et al mentioned use of paper-based methods for reporting as a logistical limitation, because it was time consuming, led to less timeliness of reporting, and was one of the issues affecting sustainability of the system [15]. They advised shifting to an online reporting platform [15]. Riccardo et al, corroborated this observation that such logistical challenges contributed to underreporting [30].
Discussion
This scoping review found minimal literature on disease surveillance for refugees in destination countries, with only 20 eligible sources included. Sources highlighted no systematic means of surveillance across migrant-receiving countries [19, 21, 30]. Few mentioned the existence of surveillance protocols and guidance necessary for accurate implementation and data sharing, while others described guidance as poorly defined or insufficient [28, 41]. Information on relevant policies shaping surveillance structures or activities was almost non-existent. Literature outside the European region appears very limited, despite significant migrant populations in the Eastern Mediterranean and North Africa since the Syrian conflict began [44].
During the significant and rapid increases in migration from war-devastated countries to Europe, ECDC emphasised the importance of establishing syndromic surveillance for refugee populations as a complement to routine national surveillance systems. Despite the presence of EU laws requiring countries to report infectious diseases, these systems have not been particularly effective [43]. In 2016, ECDC published guidance for countries on establishing their own syndromic surveillance to more quickly detect, investigate, and respond to potential epidemics in countries receiving refugees [13, 14]. This guidance and advocacy on establishing surveillance in the EU may help explain why most surveillance literature for refugees described European experiences.
Italy had the most sources on this topic and has been described by the ECDC as having an exemplary syndromic surveillance system [13, 14]. Sources describing the Italian experience provided relevant lessons about strengths and weaknesses of ad hoc surveillance in terms of fluidity of migrant populations, migration centres’ compliance, and lack of sustainability due to time and resource constraints [15]. We would encourage more countries hosting refugees to publish their surveillance experiences to help all countries identify surveillance methods, outcomes, and challenges to guide surveillance activities in future refugee responses.
Most literature on migrants and refugees focused on screening rather than surveillance systems. In some instances, infectious diseases among refugees underreported through surveillance were identified through screening [43, 45]. Rossi et al found that infectious disease reporting accuracy for migrants might be limited by their healthcare access, which other authors have reported as being restricted or challenging, though they also noted possible reporting inaccuracies in screening [17, 22, 28, 43]. This suggests disease surveillance for refugees could potentially be more effective in combination with health screening.
Another important finding in this review is the role of international organizations in surveillance activities. Our review found that UNHCR and WHO either implement new surveillance systems or support existing ones depending on country/border situations. In the absence of official surveillance, WHO or UNHCR have led on establishing surveillance systems [35, 36, 39]. Such international involvement in surveillance stems from organisational mandates to protect health globally and across borders [46, 47]. An example is WHO’s Global Outbreak and Response Network (GOARN) that deploys technical assistance to areas of need [46, 47].
Several limitations should be considered. First, scoping reviews only include sources within authors’ search capacity (e.g. accessible on databases searched or through stakeholders). Based on the authors experience in surveillance, it is likely that much of the work on this topic remains unpublished since routine activities are often not considered sufficiently interesting to publish and during humanitarian emergencies publishing may not be a priority. Further, some research might be inaccessible (e.g. due to numerous potential search terms, political sensitivities, and in many countries refugee surveillance is integrated within routine national surveillance systems). Second, this review focused on infectious diseases generally and did not include sources only describing tuberculosis and HIV surveillance. As these are the most frequently screened diseases, due to their importance and possibly the abundance of dedicated guidelines, and since a scoping review of tuberculosis screening and surveillance was recently conducted, we considered it more useful to include infectious diseases more broadly [43, 48]. Third, we did not include sources without an English abstract so useful non-English sources may have been missed [49]. Fourth, we did not include infectious disease surveillance for refugees targeting SARS-CoV-2, since we conducted this review before the start of the COVID-19 pandemic. Despite a plethora of literature on COVID-19 surveillance, this is limited when addressing vulnerable at risk populations such as refugees [50,51,52]. It would be informative to have a specified review in the future addressing implementation of surveillance activities for refugees during pandemics, in particular COVID-19. Finally, we did not assess evidence quality, as the quantity and quality of sources were insufficient to do this meaningfully.
Conclusion
This scoping review examines the scope of the literature on infectious disease surveillance for refugees at borders and in destination countries. Though this review was conducted up to July 2021, only 20 sources were found between 1999 and 2019. Surveillance systems for refugees were primarily syndromic, countries were primarily European, and little was documented on surveillance policies or protocols. Further documentation is needed to address gaps in this literature and help guide countries welcoming refugees to set up or enhance infectious disease surveillance systems accordingly.
Availability of data and materials
Data sharing is not applicable to this article, all articles used for the review are in the references section.
Abbreviations
- CARE:
-
Common Approach for Refugees
- US-CDC:
-
Centers for Disease Control (USA)
- ECDC:
-
European Centres for Disease Control
- EMBASE:
-
Excerpta Medica Database
- EU:
-
European Union
- EURO:
-
European Regional Office (WHO)
- EWAR:
-
Early Warning and Response
- IOM:
-
International Organization for Migration
- MESH:
-
Medical Subject Headings
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- UNHCR:
-
United Nations Refugee Agency
- WHO:
-
World Health Organization
References
Choi BCK. The Past , Present , and Future of Public Health Surveillance. Scientifica (Cairo). 2012;2012:26.
Thacker SB, Stroup DF. Origins and progress in surveillance systems. In: Nkuchia M. M’ikanatha, Ruth Lynfield CAVB and H de V, editor. Infectious Disease Surveillance. Blackwell Publishing Ltd; 2013. p. 21–31.
Declich S, Carter AO. Public health surveillance: historical origins, methods and evaluation. Bull World Health Organ. 1994;72(5479):285–304.
WHO. Communicable disease surveillance and response systems - Guide to monitoring and evaluating [Internet]. Epidemic and pandemic alert and response. 2006. Available from: https://www.who.int/csr/resources/publications/surveillance/WHO_CDS_EPR_LYO_2006_2.pdf
Wilken D, Baur X, Barbinova L, Preisser A, Meijer E, Rooyackers J, et al. What are the benefits of medical screening and surveillance? Eur Respir Rev. 2012;21(124):105–11.
WHO. Principles and practice of screening for disease. 1968.
Levy BS, Sidel VW. Documenting the effects of armed conflict on population health. Annu Rev Public Health [Internet]. 2016;37(1):205–18 Available from: http://www.annualreviews.org/doi/10.1146/annurev-publhealth-032315-021913.
Elias CJ, Alexander BH. Sokly TAN. Infectious Disease Control in a Long-term Refugee Camp : The Role of Epidemiologic Surveillance and Investigation. 1990;80(7):824–8.
Knudsen A. Widening the protection gap: the “politics of citizenship” for Palestinian refugees in Lebanon, 1948-2008. J Refug Stud. 2009;22(1):51–73.
Thomas SL, Thomas SDM. Displacement and health. Br Med Bull. 2004;69(February):115–27.
Eiset AH, Wejse C. Review of infectious diseases in refugees and asylum seekers-current status and going forward. Public Health Rev. 2017;38(1):1–16.
Altare C, Kahi V, Ngwa M, Goldsmith A, Hering H, Burton A, et al. Infectious disease epidemics in refugee camps: a retrospective analysis of UNHCR data (2009-2017). J Glob Heal Reports. 2019;3.
ECDC. Expert opinion on the public health needs of irregular migrants, refugees or asylum seekers across the EU’s southern and south-eastern borders. 2015; Available from: https://ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/Expert-opinion-irregular-migrants-public-health-needs-Sept-2015.pdf
ECDC. Handbook on implementing syndromic surveillance in migrant reception / detention centres and other refugee settings. 2016; Available from: http://ecdc.europa.eu/en/publications/Publications/syndromic-surveillance-migrant-centres-handbook.pdf
Napoli C, Riccardo F, Declich S, Dente MG, Pompa MG, Rizzo C, et al. An early warning system based on syndromic surveillance to detect potential health emergencies among migrants: results of a two-year experience in Italy. Int J Environ Res Public Health. 2014;11(8):8529–41.
Henning KJ. Overview of syndromic surveillance what is syndromic Surveillance ? CDC MMWR. 2004;53.
Sarma N, Ullrich A, Wilking H, Ghozzi S, Lindner AK, Weber C, et al. Surveillance on speed: Being aware of infectious diseases in migrants mass accommodations - an easy and flexible toolkit for field application of syndromic surveillance, Germany, 2016 to 2017. Eurosurveillance [Internet]. 2018;23(40):1700430. Available from: https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2018.23.40.1700430
HCDCP. Epidemiological Surveillance in points of care for refugees-migrants [Internet]. 2017. Available from: http://www.keelpno.gr/Portals/0/Αρχεία/Επιδημιολογικά δεδομένα/Επιδ Επιτ προσφύγων - μεταναστών/2018/Surveillance-refugees-weekly-EN-2018-35.pdf.
WHO-EURO. Sicily, Italy: Assessing health-system capacity to manage sudden large influxes of migrants [Internet]. 2014. Available from: http://www.euro.who.int/__data/assets/pdf_file/0007/262519/Sicily-Italy-Assessing-health-system-capacity-manage-sudden-large-influxes-migrantsEng.pdf?ua=1
WHO-EURO. Spain: assessing health system capacity to manage sudden large influxes of migrants (2018) [Internet]. 2018. Available from: http://www.euro.who.int/__data/assets/pdf_file/0004/373216/spain-report-eng.pdf
WHO-EURO. Greece: assessing health-system capacity to manage sudden large influxes of migrants [Internet]. 2015. Available from: http://www.euro.who.int/en/publications/abstracts/greece-assessing-health-system-capacity-to-manage-sudden,-large-influxes-of-migrants-2015.
Woodward A, Howard N, Wolffers I. Health and access to care for undocumented migrants living in the European Union: a scoping review. Health Policy Plan. 2014;29(7):818–30.
Ames H, Glenton C, Lewin S. Purposive sampling in a qualitative evidence synthesis: a worked example from a synthesis on parental perceptions of vaccination communication. BMC Med Res Methodol. 2019;19(26):1–9.
IOM. Key Migration Terms [Internet]. 2021 [cited 2021 Jun 12]. Available from: https://www.iom.int/key-migration-terms
UNHCR. Global trends: Forced displacement in 2020. 2021.
UNHCR. Convention and Protocol Relating to the Status of Refugees [Internet]. Vol. 10, International and Comparative Law Quarterly. 2010. Available from: http://www.unhcr.org/3b66c2aa10.pdf
Braun V, Clarke V, Hayfield N, Moller N, Tischner I. Handbook of research methods. In: Liamputtong P, editor. Health social sciences. Springer Singapore: Singapore; 2019. 2248 p.
Bozorgmehr K, Samuilova M, Petrova-Benedict R, Girardi E, Piselli P, Kentikelenis A. Infectious disease health services for refugees and asylum seekers during a time of crisis: A scoping study of six European Union countries. Health Policy (New York). 2018/04/21. 2018;
Riccardo F. Bella A. Giambi C, Del Manso M, Caporali MG, et al. Evaluation report of the CARE syndromic surveillance pilot: Zuanna TD; 2017.
Riccardo F, Rossi PG, Chiarenza A, Noori T, Declich S. Letter to the editor: responding to a call for action - where are we now? Euro Surveill. 2015;20(50):1–2.
Napoli C, Dente MG, Kärki T, Riccardo F, Rossi P, Declich S. Screening for infectious diseases among newly arrived migrants: experiences and practices in non-EU countries of the Mediterranean basin and black sea. Int J Environ Res Public Health. 2015;12(12):15550–8.
Riccardo F, Napoli C, Bella A, Rizzo C, Rota MC, Dente MG, et al. Syndromic surveillance of epidemic-prone diseases in response to an influx of migrants from North Africa to Italy, may to October 2011. Eurosurveillance. 2011;16(46):1.
Germinario C, Serena Gallone M, Tafuri S. Migrant health: the Apulian model. Epidemiol Prev. 2015;39(4):76–80.
Valenciano M, Pinto A, Coulombier D, Hashorva E, Murthi M. Surveillance of communicable diseases among the Kosovar refugees in Albania , April–June 1999. Euro Surveill. 1999;4(9).
Brusin S. The communicable disease surveillance system in the Kosovar refugee camps in the former Yugoslav Republic of Macedonia April-august 1999. J Epidemiol Community Health. 2000;54(1):52–7.
WHO. WHO Health update for Darfur, Sudan and Chad [Internet]. 2004 [cited 2018 Oct 27]. Available from: http://www.who.int/mediacentre/news/briefings/2004/mb4/en/
Amabo FC, Seukap EC, Mathieu E, Etoundi GA. Evaluation of diarrheal disease surveillance in the Minawao refugee camp , Cameroon , 2016. Int J Infect Dis [Internet]. 2019;82:9–14. Available from: https://doi.org/10.1016/j.ijid.2019.02.032.
Kouadio IK, Koffi AK, Attoh-Toure H, Kamigaki T, Oshitani H. Outbreak of measles and rubella in refugee transit camps. Epidemiol Infect [Internet]. 2009;137(11):1593–601 Available from: http://0-www.jstor.org.catalogue.libraries.london.ac.uk/stable/40272196.
WHO-SEARO. Health surveillance in Cox ’ s Bazar: WHO ’ s diseases detectives Meru Sheel , Epidemiology Team L … [Internet]. 2018 [cited 2018 Oct 26]. Available from: http://www.searo.who.int/bangladesh/surveillancecxb/en/
Turner P, Turner C, Watthanaworawit W, Carrara V, Cicelia N, Deglise C, et al. Respiratory virus surveillance in hospitalised pneumonia patients on the Thailand-Myanmar border. BMC Infect Dis. 2013;13(1).
Waterman SH, Escobedo M, Wilson T, Edelson PJ, Bethel JW, Fishbein DB. A new paradigm for quarantine and public health activities at land Borders: opportunities and challenges. Public Heal Reports [Internet]. 2009;124(2):203–11 Available from: http://0-www.jstor.org.catalogue.libraries.london.ac.uk/stable/25682196.
McCarthy AE, Weld LH, Barnett ED, So H, Coyle C, Greenaway C, et al. Spectrum of illness in international migrants seen at GeoSentinel clinics in 1997–2009, part 2: migrants resettled internationally and evaluated for specific health concerns. Clin Infect Dis. 2013;56(7):925–33 2012/12/12.
Giorgi Rossi P, Riccardo F, Pezzarossi A, Ballotari P, Dente MG, Napoli C, et al. Factors Influencing the Accuracy of Infectious Disease Reporting in Migrants: A Scoping Review. Int J Env Res Public Heal. 2017/07/06. 2017;14(7).
IFRC. Middle East and North Africa IFRC Country Office: Country Programme Overview. 2019:2019.
Tiittala P, Ristola M, Liitsola K, Ollgren J, Koponen P, Surcel H, et al. Missed hepatitis b / c or syphilis diagnosis among Kurdish , Russian , and Somali origin migrants in Finland : linking a population- based survey to the national infectious disease register. 2018;1–11.
Lazcano-Ponce E, Allen B, González CC. The contribution of international agencies to the control of communicable diseases. Arch Med Res. 2005;36(6):731–8.
Calain P. Exploring the international arena of global public health surveillance. Health Policy Plan. 2007;22(1):2–12.
WHO. Global Tuberculosis Report. 2020.
UNHCR. Figures at a Glance [Internet]. 2021. Available from: https://www.unhcr.org/figures-at-a-glance.html
Vonen HD, Olsen ML, Eriksen SS, Jervelund SS, Eikemo TA. Refugee camps and COVID-19: can we prevent a humanitarian crisis ? Scand J Public Health. 2021;49:27–8.
Kondilis E, Papamichail D, Mccann S, Carruthers E, Veizis A, Orcutt M, et al. The impact of the COVID-19 pandemic on refugees and asylum seekers in Greece : a retrospective analysis of national surveillance data from 2020. EClinicalMedicine [internet]. 2021;37:100958. Available from. https://doi.org/10.1016/j.eclinm.2021.100958.
Khan N, Mo M, Rahman M. Risks of COVID19 outbreaks in Rohingya refugee camps in Bangladesh. Public Heal Pract. 2020;1(June):1–2.
Acknowledgements
Not applicable.
Funding
None received.
Author information
Authors and Affiliations
Contributions
MS and NH conceived the study. MS collected and analysed data with inputs from other authors and drafted the manuscript with help from NH. ZF and NH revised for critical content. All authors approved the version for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
None to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Saleh, M., Farah, Z. & Howard, N. Infectious disease surveillance for refugees at borders and in destination countries: a scoping review. BMC Public Health 22, 227 (2022). https://doi.org/10.1186/s12889-022-12646-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-12646-7