- Research
- Open access
- Published:
Barriers to cervical cancer screening in Africa: a systematic review
BMC Public Health volume 24, Article number: 525 (2024)
Abstract
Introduction
Africa has one of the highest burdens of cervical cancer in the world. The unacceptably high incidence and mortality rates could be reduced through implementing a comprehensive approach to its prevention and control that includes screening, which however, is low in most low-and-middle-income countries. Hence, this systematic review aims at exploring factors that prevent women from utilising cervical cancer screening services in the region.
Methods
A mixed method systematic review was conducted. A search was performed on PubMed (Medline), EMBASE, CINAHL (EBSCOHOST) and Scopus databases for articles published until May 2019 without time, language or study design limits. Two reviewers critically appraised the included studies independently using the standard quality assessment criteria for evaluating primary research papers. Results of the quantitative and mixed methods studies were transformed into qualitative data and synthesised using thematic analysis.
Results
From a potential 2 365 studies, 24 from 11 countries met the eligibility criteria and were selected; eight qualitative, 13 quantitative, and three that used the mixed-method approach. The primary barriers were identified as poor access to screening services, lack of awareness and knowledge on cervical cancer and screening, and socio-cultural influences. Service providers perceived lack of skills, screening equipment and supplies, and staff shortages as the major barriers to the provision of screening services.
Conclusion
Barriers to cervical cancer screening in Africa are multifaceted and require a holistic approach that will address them concurrently at the health system, individual, interpersonal, community and structural levels. Political will complimented by stakeholder involvement is required in the development and implementation of strategies that will ensure acceptability, availability, accessibility, and affordability of screening to minimise barriers in accessing the service.
Introduction
Cervical cancer is the fourth most common cancer among women worldwide with an estimated 604,127 new cases and 341,831 deaths reported in 2020 [1], up from 528,000 new cases and 266,000 deaths reported in 2012 [2]. The bulk of the global burden rests with Africa, Latin America, the Caribbean and Asia where approximately 90% of deaths occur [3]. With an estimated population of 372.2 million women aged 15 years and older who are at risk of developing cervical cancer in Africa, 119, 284 women are diagnosed with cervical cancer while 81,687 die from the disease every year [4]. Compared to other regions in the world, Africa has higher cervical cancer incidence and mortality rates [1, 3, 5]. Cervical cancer screening can reduce the incidence of the disease by 70–80% if targeted appropriately [6, 7]. However, in many parts of Africa, the disease is often not identified until it reaches advanced stages that are associated with poor outcomes [8]. This has been attributed to lack of comprehensive cervical cancer screening programmes in most countries [5]. Cervical cancer is the most preventable cancer due to its slow progression and early identifiable precancerous lesions which can be treated before they progress to cancer [9] hence, women need not die from cervical cancer.
Primary studies have been conducted over the past decades to identify barriers to the uptake of cervical cancer screening in various African countries. Although limited, systematic reviews have also been done to look into challenges which women encounter in accessing cervical cancer screening services in Sub-Saharan Africa [10, 11]. Despite the recommendations that have been made for overcoming the existing barriers, evidence suggests that cervical cancer incidence rates continue to increase in Africa while declining in many developed countries [1]. A richer understanding of the reasons for the underutilisation of cervical cancer screening programmes in Africa requires further exploration. This review therefore aimed at identifying the unique contextual circumstances that prevent women from accessing cervical cancer screening in many parts of Africa. Guided by the Socio-ecological framework adopted from Kaufman and colleagues [12], our systematic review extends the knowledge already available from earlier conducted studies. Findings should guide restructuring of cervical cancer screening policies and guidelines for implementation of proactive context specific interventions that should address the structural, health system, societal, socio-economic and cultural factors at a broader level to overcome screening barriers. This could improve the uptake of screening and subsequently reduce the high cervical cancer morbidity and mortality rates in Africa. Gaps for future research will also be identified.
Methods
This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines [13].
Search strategy
We subjectively and iteratively developed a comprehensive set of search terms. In the first instance, we checked PubMed (Medline) to identify controlled vocabulary Medical Subject Headings (MeSH) terms related to cervical cancer, and additionally identified key text words based on our knowledge of the field. This yielded three key concepts; cervical cancer, screening (irrespective of screening method), and Africa. The term ‘barrier’ was not used because the concept can be described in many different ways, and we did not want to risk missing some relevant papers. Medline search terms for other electronic databases were modified to conform to their search functions. PubMed (Medline), Embase (OVID), CINAHL (EBSCOHOST) and Scopus electronic bibliographic databases were searched for articles published until May 2019 without language and study design limits. The "related citations" search key in PubMed was further used to identify similar papers. Reference lists of potentially relevant articles were checked manually for additional citations. A detailed search strategy with terminology specific to each database is included (Supplementary File 1).
Study selection
This systematic review included studies on individual, interpersonal, community, health system and structural factors that prevented women from cervical cancer screening attendance in most African countries. The selection criteria were based on original quantitative and qualitative studies that reported barriers from the perspectives of women and health providers. Studies on women with a confirmed cervical cancer diagnosis were not included in the systematic review. Grey literature and conference abstracts without full articles were also excluded. Although these could have been useful sources containing relatively new information on the research area, it is generally premised that non-peer-reviewed articles are less scientifically rigorous than those that are peer reviewed and published [14].
Our systematic review is grounded on the socio-ecological framework by Kaufman and colleagues which describes the interplay between multiple levels of influence on individual behaviour for the promotion of health [12]. The model suggests that a health outcome is determined by individual, interpersonal, institutional, community and public policy factors [15]. In this study “Barrier” refers to any factor that prevents women from accessing cervical cancer screening from any level of the socio-ecological framework and classified into five areas as follows:
Individual level barriers: These are factors at the micro-level that include personal perceptions, knowledge, beliefs and emotions.
Interpersonal barriers: These arise from influences from spouse, family and other social networks.
Community level barriers: These are a result of influences at higher levels which include traditional and cultural norms, religious beliefs and stigma.
Health system related barriers: These are factors within the health system that relate to resources and service delivery.
Structural barriers: These are factors related to policy issues and other macro-contextual factors that affect a woman’s health seeking behaviours directly.
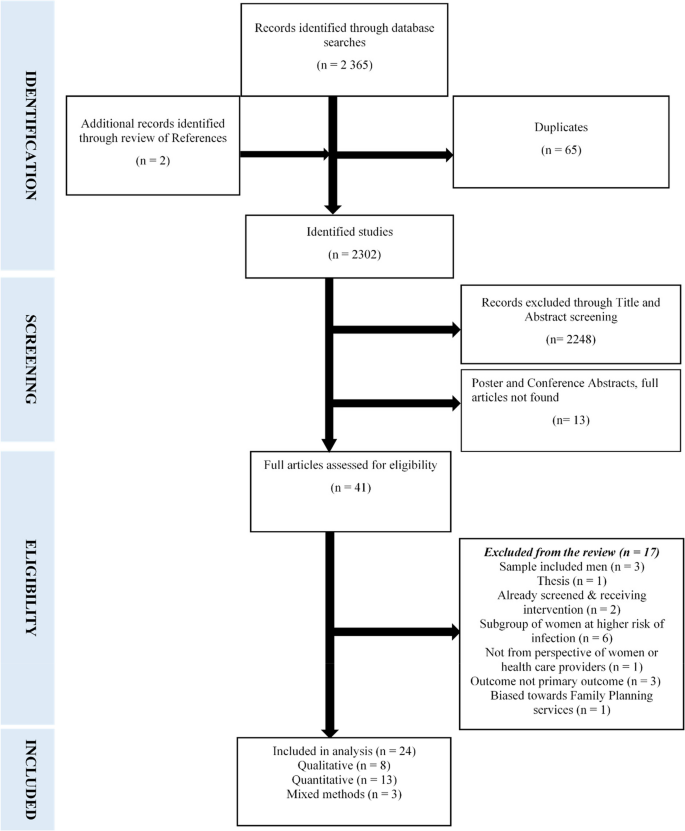
Mendeley reference manager was used to save and view titles and abstracts of all articles retrieved from the electronic databases, and to detect duplicates. Two independent reviewers (FM and VS) screened the 2 365 titles and abstracts of studies obtained through database searches. Two additional articles were identified from references after reading the full text articles (n = 2 367). Screening of articles excluded duplicates (n = 65), studies not relevant to the title (n = 2 248), and abstracts of poster and conference presentations whose full articles were not obtained (n = 13). The remaining 41 articles were reviewed in full text with 17 studies further eliminated for not meeting the inclusion criteria. The screening process resulted in the selection of 24 articles which met the eligibility criteria. Disagreements on inclusion of certain articles were resolved through discussion to reach a consensus [16]. The selection process is shown in Fig. 1.
Assessment of methodological quality
The quality of each study was evaluated by two independent reviewers (FM and VS) using the standard quality assessment criteria for evaluating primary research papers adapted from Kmet and colleagues [17]. A checklist specific to each research method required the reviewer to select either; “yes” or “no” to questions focusing on the methodological aspects of each article. This tool was appropriate for assessing the quality of the overall body of evidence given in the heterogeneous literature and helped to gauge the quality of each individual study against set standards. Qualitative studies were evaluated using the following criteria: question or objective clearly described, study design evident and appropriate, context for the study clear, connection to a theoretical framework or wider body of knowledge, sampling strategy described, relevant and justified, data collection methods clearly described and systematic, data analysis clearly described and systematic, and conclusion supported by results [17]. Quantitative studies were assessed for the following aspects: question or objective sufficiently described, study design evident and appropriate, method of subject selection described and appropriate, subject characteristics sufficiently described, sample size appropriate, analytic methods described, justified and appropriate, results reported in sufficient detail, and conclusions supported by the results [17]. The quality of studies which used the mixed methods approach was rated under the dominant method that was discussed first in that particular study.
To further determine the overall risk of bias and the quality of evidence, each reviewed article was given a quality of low, medium or high to inform the decision making. Each quality component was rated 0 to 2 based on the reviewer’s subjective assessment, with a possible least score of 0, and a maximum score of 16. A sum score of the quality components gave the overall quality rating of each article. A score of 0–8 was rated as low, 9–12 as medium and 13–16 as high. For a study to be included, it had to attain a minimum rating of medium. All the included studies fulfilled this requirement. The quality assessment for the qualitative studies is presented in Table 1.
Table 2 presents the quality assessment for the quantitative studies.
Data extraction and synthesis
A data extraction sheet was developed using the following predetermined data fields: first author, country and year of publication, title, research and data collection methods, sampling technique and sample size, and barriers identified for cervical cancer screening. One reviewer extracted the data (FM) while the second (VS) cross checked the extracted data for accuracy. Informed by the variation in the research methodologies between included studies and the multifaceted dimensions of screening barriers given, results of the quantitative and mixed methods studies were transformed into qualitative data and synthesised using thematic analysis. [16]. Data were summarised in descriptive form. A profile of all the studies included in the review highlighting the major screening barriers identified is given in Table 3.
Results
Study characteristics
The key characteristics and findings of the 24 included articles are summarised in Table 3. The studies were published between 2005 and 2019. Eight were conducted in Nigeria, three in Kenya, two each in Uganda, Ethiopia, Malawi and Zimbabwe and one each in South Africa, Burkina Faso, Tanzania, Ghana and Botswana. Eight (33.3%) studies were qualitative, thirteen (54.2%) quantitative and three (12.5%) used the mixed method approach. Sixteen (66.7%) studies evaluated barriers to cervical cancer screening from the perspective of women who are the recipients of screening and six (25%) from the perspective of health service providers. Two (8.3%) evaluated the barriers from the perspective of both women and health service providers.
Qualitative studies
Purposive sampling was used in the majority of qualitative studies (6/8, 75%). For data collection, two studies each used In-depth interviews (25%) and FGDs (25%) respectively. The remaining four each used KIIs (12.5%), interviews (12.5%), a combination of FGDs and KIIs (12.5%) and a combination of interviews and field notes (12.5) respectively.
Quantitative studies
Of the 13 quantitative studies, 5 (38.5%) used convenience sampling. Multi-stage random sampling was used in 4 (30.8%), purposive sampling in 3 (23%) and systematic sampling in 1 (7.7%) study. Interviewer administered questionnaires were used for data collection in 8 (61.5%) studies and self-administered questionnaires in four (30.8%). One (7.7%) study used both self and interviewer-administered questionnaires depending on whether the participant could read and write. The sample size of the studies ranged from 100 to 3 712 participants.
Mixed methods studies
All three studies which employed both the qualitative and quantitative approaches used the interviewer-administered questionnaire for the collection of quantitative data. For the qualitative component, in-depth interviews and FGDs were each used in two studies, respectively. The third study used document analysis, FGDs, in-depth interviews and narratives from two women with a diagnosis of cervical cancer and one who had hysterectomy done. Findings from the narratives were not used in this systematic review as they were obtained from participants who did not meet the eligibility criteria for inclusion.
Barriers to cervical cancer screening
Overall, 28 screening barriers were identified from the perspectives of service recipients, and 10 from the perspectives of service providers. Mostly cited by women were; inaccessibility of screening services, lack of awareness and knowledge on cervical cancer and screening benefits, and financial and socio-cultural constraints. Service providers perceived lack of training necessary to conduct screening, lack of equipment and supplies, staff shortages and gender and age of the health practitioner as major barriers to screening provision. Thematic analysis based on the socio-ecological framework which grounded the review yielded five a priori themes namely: health-system related, individual level, interpersonal, community related, and structural barriers. All the themes were not country-centric and could be transferrable between geographical settings in the region.
Health system related barriers to cervical cancer screening
Inaccessibility of screening services
Lack of access to screening services was identified as the key barrier to screening. Women maintained that screening services were not available at their local health facilities [23, 26, 27, 30, 32, 35, 38, 41]. The long distances they had to travel to reach the nearest screening sites usually located at tertiary levels of health care, were a deterrent to screening [18, 21, 26, 29, 30, 35, 37, 38]. This also has financial implications in terms of transport costs and lost time. Screening facilities’ operational times not amenable with women's schedules also posed a challenge and limited their chances of screening [38]. Those who had physical access to screening facilities found it difficult to navigate their way to the right place as information and directions were in most cases not readily available [25].
Service providers concurred that health facilities that provide screening were few [22] and far away from communities [23]. This resulted in women having to travel long distances to get screened, while not all facilities offered the service on a daily basis [20]. Transport to get to screening centers was also a challenge [22]. Access to screening is thus affected by unavailability of local screening facilities, transport constraints and screening operating times which are not user-sensitive.
Limited funding for cervical cancer programmes
Lack of a dedicated budget for cervical cancer programmes was highlighted as a barrier as it resulted in insufficient resources required to provide screening [40]. This included space for the provision of efficient screening services, [20, 36] and technical support to monitor the programme and provide guidance to service providers [20, 40]. Follow-up of patients who required further management also posed a challenge for health personnel, thus defeating the whole purpose of screening [26, 31].
Lack of skilled providers
Service providers maintained that shortage of personnel is a major hindrance to the uptake of screening considering that staff well equipped in the provision of the service is in short supply [20, 23, 36, 40]. Consequently the available trained personnel are not able to meet the demand [20, 26, 36]. This is also attributable to the high staff turnover among the trained cadres, [40] and lack of training opportunities for the available nurses and doctors [31]. Furthermore, trained providers are assigned to areas not related to screening, thus negatively affecting the availability of screening services [20, 40]. At some health facilities, the same personnel who provided screening were also responsible for rendering other maternal and child health services, which increases the workload and reduces their motivation [20]. Accordingly, the time within which screening sites are operational is limited due to the multiplicity of tasks skilled staff have to perform.
Lack of equipment and supplies
A general shortage of equipment and screening consumables was identified by service providers as a barrier to screening [20, 23, 30, 31, 36, 40]. Facilities often run out of supplies and cryotherapy is sometimes not provided due to broken down equipment which cannot be repaired for lack of funds [20].
Negative attitudes of service providers
Four studies; three [23, 27, 38] from the perspective of women and one [40] from the perspective of service providers highlighted negative attitudes of health personnel as an important reason for women's failure to seek screening. Women report that health workers are uncooperative and hostile to them. Such inappropriate behaviour leaves them with no option but to consult traditional healers for health care [23]. When women request screening, health workers allege to be too busy, and if the service is provided, no explanation related to the procedure is given [27]. Consistent with this, service providers argue that due to poor motivation, they lack commitment to efficiently provide the service. Such behaviours deprive women access to the screening services which they require [40].
Individual level barriers to cervical cancer screening
Lack of access to screening information
Women generally lack awareness of cervical cancer as a disease of public health concern [18, 29]. Those who may have heard about the disease have no full knowledge of its risk factors, prevention, and signs and symptoms [23, 25,26,27, 32, 33, 35, 41]. In concurrence, service providers attribute the low screening uptake to women's low levels of awareness about cervical cancer [20, 22, 40]. This consequently does not give women the motivation to seek screening. Moreover, women often have inadequate [36] and inaccurate [22] knowledge on cervical cancer and screening [23,24,25, 29, 32, 33, 37]. Regrettably, some women lack information on the existence of screening programmes even where such services are available locally [26], are not aware of the location of screening sites [18, 23, 28,29,30, 33, 35, 41], the appropriate age for screening [38, 41], and the need and benefits of screening [26, 27]. This dearth of information is partly due to poor information dissemination by health workers as indicated by both service recipients [18, 33, 41] and service providers including private practitioners [19], and absence of relevant health educational programmes [35]. In addition, service providers have highlighted that health professionals especially at the lower levels of care lack adequate knowledge on cervical cancer and its prevention and control and are therefore not able to give women up to date screening related information [22].
Financial constraints
Lack of financial resources was reported as a common obstacle to participation in cervical cancer screening. The cost of the test was considered as expensive by some women [23, 27, 28, 35] and service providers [19, 22, 31]. This is partly linked to the hidden costs associated with screening since the service is offered for free in most public health facilities. The indirect costs include high transport charges to screening sites [21, 23, 25, 27, 30], time lost on travel, [21, 25] long waiting times before screening [25, 30, 36] which could have been used productively, and lack of money to pay for treatment should the screen test yield a positive result [22].
Attitude of indifference to screening
The perception that screening is unnecessary [28] and not important [18] was noted as an impediment to screening. Women see no benefit in early detection measures as they believe that one would not be cured anyway, and still die of cancer [27]. Women also suggested that they had never thought about screening [28] and therefore were not ready for the test [30], or had no interest in getting screened [32]. These negative attitudes could be emanating from their lack of symptoms [26, 28, 34, 37, 41] which instils a notion of good health and therefore finding no reason to get screened. Women also believed they were not at risk for cervical cancer [18, 25, 33, 39], while some were not aware of their being at risk for the disease [29] and therefore felt no need for screening.
Fear of procedure and outcome
Fear of pain during the procedure was identified as a screening deterrent [23, 24, 35, 38]. Women receive negative information from friends [27], or have themselves had bad screening experiences and therefore avoid repeat screens [23]. Service providers also reported that women are not comfortable with pelvic examinations and fear that insertion of the speculum causes pain, hence will not participate in screening [22, 36]. For some women, fear of the possibility of receiving a positive result was a barrier [18, 21, 23,24,25, 29, 35, 37, 38]. Finding bliss in ignorance was associated with; fear of being left by spouse if known to have cervical cancer as that was thought to interfere with sexual relations [23], fatalistic view of cervical cancer, therefore finding it better not to know [18, 21, 24, 29, 37], fear of disclosure of results which may result in stigmatisation [24], fear of the side effects of treatment [35] and worry which may lead to an early death [38]. Women also expressed fear of contracting other diseases from the screening equipment and finding out their Human immunodeficiency virus (HIV) status if cervical cancer screening was linked to HIV screening [23].
Interpersonal barriers to cervical cancer screening
Lack of spousal support
Spousal or male partner support was found to be an important factor in the practice of screening because of the patriarchal nature of the African society. Husbands were revealed to have an influence on the decision for screening [38]. Women require their husbands’ permission to get screened for financial and cultural reasons [24] and since some men do not understand the importance of screening [26], they refuse to give their consent [35]. Women get accused of being promiscuous if they express their wish to screen because of the association of cervical cancer with a sexually transmitted virus [27]. Men can thus be a hindrance to screening. Service providers confirmed men’s lack of emotional and financial support for screening [22] expressed by women [26, 27, 35, 38]. Lack of male support for screening also creates barriers to treatment adherence if the woman has a positive result [20].
Misconceptions about cervical cancer
Negative connotations linked to cervical cancer and screening within women’s social circles has been identified as a big barrier to screening. The misconception that cervical cancer is associated with promiscuity deters women from screening as they do not want to be labelled as being promiscuous [38]. Additionally, women are misinformed and made to believe that use of the speculum during the test enlarges the vagina [20], that the uterus is pulled out for examination and reinserted after screening [20, 25], and that they may not be able to have children after screening. Subsequently, they get discouraged from utilising the service. Women’s screening behaviour is thus often subject to the influence of family and friends.
Community-related barriers to cervical cancer screening
Family responsibilities
Six studies revealed that women lacked time to attend screening due to family responsibilities. As household managers whom society expects to place the wellbeing of the family before their own, women have many competing priorities related to family survival which deprive them of time for screening [18, 26]. They are too busy with household chores to go to health facilities for preventive health services [25, 27, 30] relative to curative care. Some have no household help and find it hard to leave their tasks unattended since the time it takes to complete the screening processes is long [27, 38].
Socio-cultural and religious beliefs
It is very difficult to clearly distinguish between cultural and religious considerations as these two are intricately related. The same factors reported by some women as religious were reported as cultural by others. Consequently, socio-cultural and religious beliefs and gender and age of service provider cannot be discussed independently of each other.
Some women consider participation in cervical cancer screening as inappropriate and against their cultural and religious beliefs [35]. African women are generally conservative and suffer embarrassment at lying on their backs with their legs open [22, 26] and exposing their private parts for examination [22, 27, 35], especially if it is a male providing the service [21]. Exposure of genitals is viewed as a violation of women’s privacy [37]. The cultural and religious norms which some women value discourage them from exposing their intimate body parts to other people other than their husbands, unless if there are compelling reasons [24]. Modesty, embarrassment and religious beliefs are thus significant barriers to the utilisation of screening services.
Gender and age of the service provider were seen to pose a cultural barrier to participation in cervical cancer screening programmes. Women feel ashamed, shy, embarrassed, anxious and uncomfortable if males provide the service [23, 24, 26, 27]. Service providers echoed that gender of the provider interfered with screening programmes as women do not like their private parts exposed to male practitioners particularly if they have no gynaecological problems [19, 20, 22, 36]. Furthermore, older women are not willing to be screened by younger male health workers who they consider as their sons [19, 20, 22, 23, 26]. This is attributed to cultural norms. The same sentiments in relation to gender and age of service provider are obtaining in the private sector [19].
Social stigma associated with cervical cancer and screening
One study revealed that women decline cervical cancer screening because of the stigma associated with having cervical cancer [21]. They avoid going to screening sites because people may think they have the disease and suffer societal rejection. Stigma related to misconceptions was again mentioned by service providers as one of the perceived patient factors that inhibit screening uptake [36].
Structural barriers
Over and above the health system, individual, interpersonal and community related barriers to screening, clear comprehensive cervical cancer management policies and guidelines to guide cervical cancer screening and systematic cervical cancer screening programmes are not readily available in the region [26, 30, 40]. Efforts to prevent cervical cancer are therefore haphazard, and this has a negative impact on screening [26]. Where available, the policies are weak and characterised by a lack of political will and backing by governments. Inadequate funding of the programme results in poor availability of all resources necessary for screening due to the low priority which cervical cancer screening is given within the health system [40].
Suggested strategies for addressing barriers to cervical cancer screening
Women and health service providers mutually suggest that; increasing access to cervical cancer screening within communities by addressing transport challenges [23], creating and raising awareness on screening through community mobilisation and sensitisation [20, 23, 26], assigning female staff to conduct screening [23], availing more skilled staff and supplies for the screening programme, and a collaborative approach at crafting policies that accord screening priority like other maternal and child health programmes [35], would improve the uptake of screening.
Discussion
This systematic review synthesised findings of the key barriers to the uptake of cervical cancer screening from 24 studies conducted in 11 African countries. The barriers were presented from the viewpoint of service recipients and providers. Our analysis across the included studies indicate lack of information on the importance of screening and poor access to screening services as the most predominant barriers to cervical cancer screening in the region. Concordance of themes was demonstrated between qualitative and quantitative studies, and between women and service providers’ perspectives. Triangulation of findings was thus achieved [42].
Based on the findings of this review, factors that negatively impact cervical cancer screening in Africa are multidimensional and although common between countries, vary in magnitude from one setting to another. At the level of the health system, restricted access to screening in particular; lack of local health facilities that provide screening services, and prohibitive distances and cost to screening sites were shown to be the biggest challenges in the uptake of screening. The findings compare well with other studies conducted among indigenous populations worldwide [7], in Sub-Saharan Africa [10], in the Pacific [43] and in other middle and upper- middle income countries such as Turkey, Thailand, Jamaica and China which also report poor access to screening services due to various structural and health system related factors[44].
Most reviewed studies have advanced relatively similar recommendations for addressing the barriers to cervical cancer screening at different time periods yet, the uptake of screening has only slightly improved overtime. Our study attributes this to the fragmented tackling of the socio-ecological framework linked barriers independently of each other, and postulates that responding to challenges at only one level of the framework has the effect of increasing the barriers at a different ignored level. For example; increasing awareness and knowledge on screening among women has the likelihood of increasing the demand for the service. However, if screening facilities are not concurrently increased, the challenge will shift from the demand to the supply side. Our review further hypothesises that even if all other barriers could be addressed, screening incidence would still remain low if screening facilities are not universally rolled out to communities. Evidenced to this is the effective screening programmes in high-income countries that have resulted in low cervical cancer incidence [45]. Access to services is central to screening uptake in view of the fact that women cannot engage in cervical cancer screening if there are no services to deliver it [43]. This therefore requires the development of context specific innovative policies and strategies, or the modification of existing ones to make the service readily accessible to all women who need it.
One long term solution which has been recommended in previous studies but has not been universally applied is the inclusion of cervical cancer prevention and control into the nurses’ pre-service training curriculum [43, 46]. Our study further recommends that the cervical cancer component be examinable both theoretically and practically to ensure nurses would have acquired the necessary skills upon completion of their training. This is because nurses constitute the most authoritative source of health information especially for women [47] and are available at all levels of health care. To address the associated financial constraints which have been raised as prohibitive to this recommendation, the training could make use of the already existing resources since all teaching hospitals are likely to have screening units. Screening coverage would consequently be ensured at all levels of health care given the availability of other necessary resources, which may however not be readily available in all settings in the short term. However, women would still benefit from receiving accurate information on cervical cancer prevention and control to enable them to seek screening services where available,
The World Health Organization has also provided guidelines on the attainment of universal screening coverage, its scalability and sustainability [48], which African countries need to modify and implement. Furthermore, the World Health Organization states that the success of the drive to eliminate cervical cancer depends on political will and country-led action investments [49]. This is particularly required in African countries for the economic support of cervical cancer screening programmes and development or more effective implementation of country-centric policies and guidelines for screening. Nevertheless, individual and interpersonal factors within the socio-ecological model still need to be addressed given that some low resource countries in Africa with a strong political will still report low screening rates [50]. Considering alternative screening delivery models like mobile clinics is another viable option that has proved to be effective in other low resource settings [46]. This should be strengthened or implemented in settings that have not introduced it.
Lack of awareness and knowledge about cervical cancer and screening was commonly reported in this review although not identified as the primary barrier to screening, contrary to findings from previously conducted reviews [9, 10, 43, 44, 51, 52]. This variance could be a result of on-going awareness campaigns and improved education of women about the disease and its prevention, which could be an indication that knowledge about cervical cancer and screening is progressively improving. The limited knowledge that women have on cervical cancer and screening has been linked to failure by health professionals to educate their communities appropriately. A number of studies conducted in similar settings have reported similar findings [9, 11, 43]. Effective health education is likely to improve women’s knowledge about the disease and enhance the uptake of screening [15, 33]. Facilitation of intrinsic motivation through establishing systems for continuing knowledge and skills training of health professionals in cervical cancer prevention could help in the scale up of screening coverage to address this gap. More opportunities for the education of communities including men need to be explored in a culturally competent manner using affordable and available resources. Community Health Workers for example, possess authority and influence and are respected in their communities. Such authoritative sources of cultural knowledge could be harnessed and trained to complement the efforts of health professionals in disseminating knowledge on cervical cancer screening. A clearer understanding and increased knowledge among women could dispel myths and misconceptions about cervical cancer and screening and could result in an increased demand for the service. For women to participate in screening, they need to have knowledge of the disease and how it is screened [43]. As stated by some women; “it is not possible to use what they don’t know about” [18].
Our review identified that at the interpersonal and community levels of the socio-ecological model, women are essentially constrained from screening by cultural and religious factors. This finding is consistent with other studies which confirm that women need to seek approval and funding from their spouses or partners to enable them to access cervical cancer screening [15]. Such approval is at times denied for varying reasons [11, 44, 52, 53]. Moreover, women may also be discreet in discussing reproductive health issues with their spouses for cultural reasons [46], while husbands are not expected to be involved in talking about women’s health issues [11, 54]. Male involvement in reproductive health services needs further support to enhance women's attendance for screening.
The provision of screening services by males has been seen to discourage women, particularly the older ones, from seeking screening. Findings of this review are congruent with evidence from other studies [15, 53, 55, 56]. For some cultures, it is taboo foe females to expose their nudity to males other than their sexual partners and is contradictory to their and values [10]. On the contrary, some studies conducted among minority groups in Canada revealed that women felt uncomfortable discussing or undertaking the screening test irrespective of the sex of the service provider [9]. The differences in findings could be related to cultural beliefs.
However, despite the religious taboos and social stigmas associated with screening, women still respect health providers’ opinions and recommendations [9]. This reiterates the critical role health workers have in educating women on cervical cancer and screening at every interaction with women for enhanced utilisation of screening services. Evidently, there is a need to change some socio-cultural beliefs if uptake of screening is to increase. This however is a challenging task since women’s understanding of issues is grounded on religious and cultural traditions and makes promotion of screening difficult to address in isolation to those traditions [52]. Accordingly, a simple educational intervention is unlikely to achieve the desired result. Rather than targeting just the women with cervical cancer screening messages, educational interventions should target all levels of the socio-ecological framework and be extended to include families, communities and traditional/religious leaders who could serve as change agents in support of promotive and preventive health programmes that include cervical cancer screening.
Limitations
Although the search strategy was tailored for studies on barriers to cervical cancer screening conducted in Africa, this was not achievable as no articles were retrieved from North and Central African countries. Screening barriers unique to these countries were therefore not explored. Evidence suggests that cervical cancer is uncommon in Northern Africa [3] which could be the reason for lack of research in that area. Nevertheless, findings of this review exclude an important segment of the study population which could be having unique barriers to cervical cancer screening. In addition, grey literature which could have provided useful insights for the review was excluded. Despite these limitations, the overall findings were consistent across the studies and can be extrapolated to similar geographical settings in Africa.
Conclusions
In this systematic review, we thematically explored the factors that prevent women from seeking cervical cancer screening services in Africa. Barriers to screening were found to be multi-dimensional spanning all levels of the socio-ecological framework. Poor access to screening facilities, lack of comprehensive knowledge on cervical cancer and screening, and socio-cultural influences were found to be the key factors that contribute to the sub-optimal uptake of cervical cancer screening among women in African countries. From the view of health personnel, trained service providers were insufficient to meet the demand for screening. Similarly, screening equipment is not adequate for the delivery of a comprehensive service.
While women could have the essential knowledge on cervical cancer and get the motivation for screening, geographical, social and financial inaccessibility of the service could prevent them from screening. Conversely, women with full understanding of screening benefits and easy access to screening may still fail to utilise the service if they find it unacceptable due to intrapersonal and community influences related to religion and culture, and health system factors. Our study elucidates the criticality of tackling the barriers to screening at all levels of the socio-ecological model in a structured manner that would prevent increasing barriers at another level in the process.
Success at achieving a high uptake of screening should therefore focus on concurrently addressing all screening barriers at the individual, interpersonal, community, health systems and structural levels and apply the primary health care model which supports the availability, accessibility, acceptability and affordability of services with full community involvement. Application of this holistic approach could provide solutions that are responsive to communities and health services’ needs. There is also a need for dedicated cervical cancer programmes budgets to make available all the required resources for screening. Our review provides insights into the need for long-term strategies to reduce screening barriers at all levels of the socio-ecological model based on the needs of the community for achieving and sustaining high screening rates. Further research is required to investigate the feasibility and cost effectiveness of this multifaceted approach.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre L, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide : Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86.
Vaccarella S, Laversanne M, Ferlay J, Bray F. Cervical cancer in Africa, Latin America and the Caribbean and Asia: Regional inequalities and changing trends. Int J Cancer. 2017;141(10):1997–2001.
Bruni L, Albero G, Serrano B, Mena M, Go’mez D, Munoz J, Bosch FX, de Sanjose S. ICO/ IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Africa. Summary Report 17 June 2019. [cited 2020 Feb 13]. Available from: https://hpvcentre.net/statistics/reports/XFX.pdf.
Akinyemiju TF, Mcdonald JA, Lantz PM. Health care access dimensions and cervical cancer screening in South Africa : analysis of the world health survey. BMC Public Health. 2015;15:382.
Victor Manuel VH. Screening and Prevention of Cervical Cancer in the World. Journal of Gynaecological Research and Obstetrics. 2017;3(3):86–92.
Kolahdooz F, Jang SL, Corriveau A, Gotay C, Johnston N, Sharma S. Knowledge, attitudes, and behaviours towards cancer screening in indigenous populations : a systematic review. Lancet Oncology. 2014;15:e504–16.
World Health Organization. Cervical cancer common amongst African women. 2020. [cited 2021 Feb 15]. Available from: https://www.afro.who.int/news/cervical-cancer-common-amongst-african-women.
Ferdous M, Lee S, Goopy S, Yang H, Rumana N, Abedin T, et al. Barriers to cervical cancer screening faced by immigrant women in Canada: a systematic scoping review. BMC Women’s Health. 2018;18(1):165.
McFarland DM, Gueldner SM, Mogobe KD. Integrated Review of Barriers to Cervical Cancer Screening in Sub-Saharan Africa. J Nurs Scholarsh. 2016;48(5):490–8.
Lim JNW, Ojo AA. Barriers to utilisation of cervical cancer screening in Sub Sahara Africa: a systematic review. Eur J Cancer Care (Engl). 2017;26(1). https://doi.org/10.1111/ecc.12444.
Kaufman MR, Cornish F, Zimmerman RS, Johnson BT. Health Behavior Change Models for HIV Prevention and AIDS Care : Practical Recommendations for a Multi-Level Approach. J Acquir Immune Defic Syndr. 2014;66:250–8.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. https://doi.org/10.1136/bmj.b2700.
Scherer R, Saldanha I. How should systematic reviewers handle conference abstracts? A view from the trenches. Syst Rev. 2019;8(1):4–9.
Binka C, Nyarko SH, Awusabo-Asare K, Doku DT. Barriers to the Uptake of Cervical Cancer Screening and Treatment among Rural Women in Ghana. Biomed Res Int. 2019;2019:6320938. https://doi.org/10.1155/2019/6320938.
Musa J, Achenbach CJ, O’Dwyer LC, Evans CT, McHugh M, Hou L, et al. Effect of cervical cancer education and provider recommendation for screening on screening rates : A systematic review and meta-analysis. PLoS OneS ONE. 2017;12(9):e0183924.
Kmet LM, Lee RC, Cook LS. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Edmonton: Alberta Heritage Foundation for Medical Research (AHFMR). AHFMR - HTA Initiative #13. 2004.
Ndikom CM, Ofi BA. Awareness, perception and factors affecting utilization of cervical cancer screening services among women in Ibadan, Nigeria: a qualitative study. Reprod health. 2012;9:11.
Mookeng MJ, Mavundla TR, McFarland DM. Barriers to cervical cancer screening within private medical practices in Soshanguve, South Africa. Africa Journal of Nursing & Midwifery. 2010;12(1):27–38.
Munthali AC, Ngwira BM, Taulo F. Exploring barriers to the delivery of cervical cancer screening and early treatment services in Malawi : some views from service providers. Patient Prefer Adherence. 2015;9:501–8.
Oketch SY, Kwena Z, Choi Y, Adewumi K, Moghadassi M, Bukusi EA, et al. Perspectives of women participating in a cervical cancer screening campaign with community-based HPV self-sampling in rural western Kenya: a qualitative study. BMC Womens Health. 2019;19(1):75.
Mwaka AD, Wabinga HR, Mayanja-Kizza H. Mind the gaps: a qualitative study of perceptions of healthcare professionals on challenges and proposed remedies for cervical cancer help-seeking in post conflict northern Uganda. BMC Fam Pract. 2013;14:193.
Ndejjo R, Mukama T, Kiguli J, Musoke D. Knowledge, facilitators and barriers to cervical cancer screening among women in Uganda: A qualitative study. BMJ Open. 2017;7:e016282.
Modibbo FI, Dareng E, Bamisaye P, Jedy-Agba E, Adewole A, Oyeneyin L, et al. Qualitative study of barriers to cervical cancer screening among Nigerian women. BMJ Open. 2016;
Fort VK, Makin MS, Siegler AJ, Ault K, Rochat R. Barriers to cervical cancer screening in Mulanje, Malawi : a qualitative study. Patient Prefer Adherence. 2011;5:125–31.
Mangoma JF, Chirenje MZ, Chimbari MJ, Chandiwana SK. An assessment of rural women’s knowledge, constraints and perceptions on cervical cancer screening: the case of two districts in Zimbabwe. Afr J Reprod Health. 2006;10(1):91–103.
Ngugi CW, Boga H, Muigai AWT, Wanzala P, Mbithi JN. Factors Affecting Uptake of Cervical Cancer Early Detection Measures Among Women in Thika. Kenya Health Care for Women International. 2012;33(7):595–613.
Nwankwo KC, Aniebue UU, Aguwa EN, Anarado AN, Agunwah E. Knowledge attitudes and practices of cervical cancer screening among urban and rural Nigerian women : a call for education and mass screening. European Journal of Cancer CareJournal of Cancer Care. 2011;20:362–7.
Compaore S, Ouedraogo C, Koanda S, Haynatzki G, Chamberlain R, Soliman A. Barriers to Cervical Cancer Screening in Burkina Faso: Needs for Patient and Professional Education. J Cancer Educ. 2016;31(4):760–6.
Tarwireyi F. Perceptions and barriers to cervical cancer screening in a rural district of Mutoko, Mashonaland East Province. Zimbabwe Cent Afr J Med. 2005;51(11/12):120–2.
Kress CM, Sharling L, Owen-Smith AA, Desalegn D, Blumberg HM, Goedken J. Knowledge, attitudes, and practices regarding cervical cancer and screening among Ethiopian health care workers. Int J Womens Health. 2015;7:765–72.
Abiodun OA, Fatungase OK, Olu-Abiodun OO, Idowu-Ajiboye BA, Awosile JO. An assessment of women’s awareness and knowledge about cervical cancer and screening and the barriers to cervical screening in Ogun State, Nigeria. Journal of Dental and Medical Sciences. 2013;10(3):52–8.
Okunowo A, Daramola E, Soibi-Harry A, Ezenwankwo F, Kuku J, Okunade K, et al. Women’s knowledge of cervical cancer and uptake of Pap smear testing and the factors influencing it in a Nigerian tertiary hospital. Journal of Cancer Research and Practice. 2018;5:105–11.
Perng P, Perng W, Ngoma T, Kahesa C, Mwaiselange J, Merajver SD, et al. Promoters of and barriers to cervical cancer screening in a rural setting in Tanzania. Int J Gynaecol Obstet. 2013;123(3):221–5.
Ebu NI, Mupepi SC, Siakwa MP, Sampselle CM. Knowledge, practice, and barriers toward cervical cancer screening in Elmina, Southern Ghana. International Journal of Women’s Health. 2015;7:31–9.
Rosser JI, Hamisi S, Njoroge B, Huchko MJ. Barriers to Cervical Cancer Screening in Rural Kenya: Perspectives from a Provider Survey. J Community Health. 2015;40(4):756–61.
Chigbu CO, Aniebue U. Why Southeastern Nigerian Women Who Are Aware of Cervical Cancer Screening Do Not Go for Cervical Cancer Screening. Int J Gynecol Cancer. 2011;21(7):1282–6.
Titiloye MA, Womitenren YT, Arulogun OS. Barriers to utilization of cervical cancer screening services among women of reproductive age in Ondo, Southwest Nigeria. Afr J Biomed Res. 2017;20(3):229–35.
Ibekwe CM, Hoque ME, Ntuli-Ngcobo B. Perceived barriers of cervical cancer screening among women attending Mahalapye district hospital, Botswana. Arch Clin Microbiol. 2011;2(1).
Abiodun O, Olu-abiodun O, Ode I, State O. The understanding and perception of service providers about the community- based cervical screening in Nigeria Volume. Annals of Tropical Medicine & Public Health. 2014;6(6):637–43.
Getachew S, Getachew E, Gizaw M, Ayele W, Addissle A, Kantelhardt EJ. Cervical cancer screening knowledge and barriers among women in Addis Ababa, Ethiopia. PLos ONE. 2019;14(5):e0216522.
Heale R, Forbes D. Understanding triangulation in research. Evidence-based Nursing Evid Based Nurs. 2013;16(4):98.
Elia CR, Devine S. Barriers and enablers for cervical cancer screening in the Pacific : A systematic review of the literature. Pacific Journal of Reproductive Health. 2018;1(7):371–82.
Devarapalli P, Labani S, Nagarjuna N, Panchal P. Barriers affecting uptake of cervical cancer screening in low and middle income countries : A systematic review. Indian J Cancer. 2018;55(55):318–26.
Dykens JA, Smith JS, Demment M, Marshall E, Schuh T, Peters K, et al. Evaluating the implementation of cervical cancer screening programs in low-resource settings globally: a systematized review. Cancer Causes Control. 2020;31(5):417–29.
Mutyaba T, Faxelid E, Mirembe F, Weiderpass E. Influences on uptake of reproductive health services in Nsangi community of Uganda and their implications for cervical cancer screening. Reprod Health. 2007;4:4.
Ifemelumma CC, Anikwe CC, Okorochukwu BC, et al. Cervical Cancer Screening: Assessment of Perception and Utilization of Services among Health Workers in Low Resource Setting. Int J Reprod Med. 2019. https://doi.org/10.1155/2019/6505482.
World Health Organization. Comprehensive Cervical Cancer Control: A guide to essential practice. Second Edition. 2014.
Global strategy to accelerate the elimination of cervical cancer as a public health problem. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO.
Binagwaho A, Ngabo F, Wagner CM, Mugeni C, Gatera M, Nutt CT, et al. Integration of comprehensive women’s health programmes into health systems: cervical cancer prevention, care and control in Rwanda. Bull World Health Organ. 2013;91(9):697–703.
Islam RM, Billah B, Hossain MN, Oldroyd J. Barriers to Cervical Cancer and Breast Cancer Screening Uptake in Low-Income and Middle-Income Countries : A Systematic Review. Asian Pac J Cancer Prev. 2017;18(7):1751–63.
Anderson de Cuevas RM, Saini P, Roberts D, Beaver K, Chandrashekar M, Jain A, et al. A systematic review of barriers and enablers to South Asian women ’ s attendance for asymptomatic screening of breast and cervical cancers in emigrant countries. BMJ Open. 2018;8:e020892.
Lunsford NB, Ragan K, Lee Smith J, Saraiya M, Aketch M. Environmental and Psychosocial Barriers to and Benefits of Cervical Cancer Screening in Kenya. Oncologist. 2017;22:173–81.
Njoku A, Ngome E. Challenges faced by older women in Botswana in accessing services that address sexual and reproductive health, and family planning needs. South African Family Practice. 2013;55(3):281–8.
Onyenwenyi AOC, Mchunu GG. Barriers to cervical cancer screening uptake among rural women in South West Nigeria: A qualitative study. South African Journal of Obstetrics and Gynaecology. 2018;24(1):22–6.
Williams M, Kuffour G, Ekuadzi E, Yeboah M, ElDuah M, Tuffour P. Assessment of psychological barriers to cervical cancer screening among women in Kumasi, Ghana using a mixed methods approach. Afr Health Sci. 2013;13(4):1054–61.
Acknowledgements
This article is a component of a dissertation titled " Barriers to cervical cancer screening in Gwanda district, Zimbabwe: A mixed method analysis'' which is in the Stellenbosch University repository for dissertations. Available at: https://scholar.sun.ac.za/handle/10019.1/125887?show=full
Funding
This study is not supported by any funding body.
Author information
Authors and Affiliations
Contributions
FM conceptualised the study, developed the review protocol, screened retrieved articles, extracted and analysed the data, and wrote the first draft of the manuscript.
VS supervised the study, screened retrieved articles, validated the data analysis and critically reviewed and made revisions to the manuscript.
YT supervised the study and critically reviewed and made revisions to the manuscript.
All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to particpate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mantula, F., Toefy, Y. & Sewram, V. Barriers to cervical cancer screening in Africa: a systematic review. BMC Public Health 24, 525 (2024). https://doi.org/10.1186/s12889-024-17842-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-17842-1