- Research
- Open access
- Published:
Arts and creativity interventions for improving health and wellbeing in older adults: a systematic literature review of economic evaluation studies
BMC Public Health volume 23, Article number: 2496 (2023)
Abstract
Background
As the population ages, older people account for a larger proportion of the health and social care budget. A significant body of evidence suggests that arts and creativity interventions can improve the physical, mental and social wellbeing of older adults, however the value and/or cost-effectiveness of such interventions remains unclear.
Methods
We systematically reviewed the economic evidence relating to such interventions, reporting our findings according to PRISMA guidelines. We searched bibliographic databases (MEDLINE, EMBASE, Econlit and Web of Science and NHSEED), trial registries and grey literature. No language or temporal restrictions were applied. Two screening rounds were conducted independently by health economists experienced in systematic literature review. Methodological quality was assessed, and key information extracted and tabulated to provide an overview of the published literature. A narrative synthesis without meta-analysis was conducted.
Results
Only six studies were identified which provided evidence relating to the value or cost-effectiveness of arts and creativity interventions to improve health and wellbeing in older adults. The evidence which was identified was encouraging, with five out of the six studies reporting an acceptable probability of cost-effectiveness or positive return on investment (ranging from £1.20 to over £8 for every £1 of expenditure). However, considerable heterogeneity was observed with respect to study participants, design, and outcomes assessed. Of particular concern were potential biases inherent in social value analyses.
Conclusions
Despite many studies reporting positive health and wellbeing benefits of arts and creativity interventions in this population, we found meagre evidence on their value or cost-effectiveness. Such evidence is costly and time-consuming to generate, but essential if innovative non-pharmacological interventions are to be introduced to minimise the burden of illness in this population and ensure efficient use of public funds. The findings from this review suggests that capturing data on the value and/or cost-effectiveness of such interventions should be prioritised; furthermore, research effort should be directed to developing evaluative methods which move beyond the confines of current health technology assessment frameworks, to capture a broader picture of ‘value’ more applicable to arts and creativity interventions and public health interventions more generally.
PROSPERO registration
CRD42021267944 (14/07/2021).
Background
The number and proportion of older adults in the population has increased in virtually every country in the world over past decades [1]. In 2015, there were around 901 million people aged 60 years and over worldwide, by 2030, this will have increased to 1.4 billion [2]. An ageing population is one of the greatest successes of public health but it has implications for economies in numerous ways: slower labour force growth; working-age people will have to make greater provisions in welfare payments for older people who are no longer economically active; provisions for increased long-term care; and, society must adjust to the changing needs, expectations and capabilities of an expanding group of its citizens.
The Covid-19 pandemic shone an uncompromising light on the health and social care sector, highlighting the seriousness of gaps in policies, systems and services. It also focused attention on the physical and mental health consequences of loneliness and social isolation. To foster healthy ageing and improve the lives of older people, their families and communities, sustained and equitable investment in health and wellbeing is required [3]. The prevailing model of health and social care which is based ostensibly on formal care provision is unlikely to be sustainable over the longer term. New models, which promote healthy ageing and recognise the need for increasing reliance on self-care are required, as will be evidence of their effectiveness, cost-effectiveness and scalability.
Arts and creativity interventions (ACIs) can have positive effects on health and well-being, as several reviews have shown [4, 5]. For older people, ACI’s can enhance wellbeing [6,7,8,9], quality of life [10, 11] and cognitive function [12,13,14,15,16]. They can also foster social cohesion [17,18,19] and reduce social disparities and injustices [20]; promote healthy behaviour; prevent ill health (including enhancing well-being and mental health) [21,22,23,24,25], reducing cognitive decline [26, 27], frailty [28,29,30,31,32,33] and premature mortality [34,35,36,37,38]); support people with stroke [39,40,41,42]; degenerative neurological disorders and dementias and support end of life care [43, 44]. Moreover, ACIs can benefit not only individuals, but also others, such as supporting the well-being of formal and informal carers, enriching our knowledge of health, and improving clinical skills [4, 5].
The benefits of ACIs have also been acknowledged at a governmental level by those responsible for delivering health and care services: The UK All-Party Parliamentary Special Interest group on Arts, Health and Wellbeing produced a comprehensive review of creative intervention for health and wellbeing [45]. This report contained three key messages: that the arts can keep us well, aid recovery and support longer better lived lives; they can help meet major challenges facing health and social care; and that the arts can save money for the health service and social care.
Despite robust scientific evidence and governmental support, no systematic literature review has collated the evidence with respect to the value, cost or cost-effectiveness of such interventions. Our objective was to assess the economic impact of ACIs aimed at improving the health and wellbeing of older adults; to determine the range and quality of available studies; identify gaps in the evidence-base; and guide future research, practice and policy.
Methods
A protocol for this review was registered at PROSPERO, an international prospective register of systematic reviews (Registration ID CRD42021267944). We used pre-determined criteria for considering studies to include in the review, in terms of types of studies, participant and intervention characteristics.
The review followed the five-step approach on how to prepare a Systematic Review of Economic Evaluations (SR-EE) for informing evidence-based healthcare decisions [46,47,48]. Subsequent to developing and registering the protocol, the International Society for Pharmacoeconomic Outcomes and Research (ISPOR) published a good practice task force report for the critical appraisal of systematic reviews with costs and cost-effectiveness outcomes (SR-CCEOs) [49]. This was also used to inform the conduct of this review.
Eligibility criteria
Full economic evaluations are regarded as the optimal type of evidence for inclusion in a SR-EE [46], hence cost-minimisation analyses (CMA), cost-effectiveness analyses (CEA), cost-utility analyses (CUA) and cost–benefit analyses (CBA) were included. Social value analyses were also included as they are frequently used to inform decision-making and commissioning of services within local government. Additionally, they represent an important intermediate stage in our understanding of the costs and consequences of public health interventions, where significant challenges exist with regard to performing full evaluations [50,51,52,53].
Development of search strategies
The population (P), intervention (I), comparator (C) and outcomes (O) (PICO) tool provided a framework for development of the search strategy. Studies were included if participants were aged 50 years or older (or if the average age of the study population was 50 years or over). Interventions could relate to performance art (dance, singing, theatre, drama etc.), creative and visual arts (painting, sculpture, art making and design), or creative writing (writing narratives, poetry, storytelling). The intervention had to be active (for example, creating art as opposed to viewing art; playing an instrument as opposed to listening to music). The objective of the intervention had to be to improve health and wellbeing; it had to be delivered under the guidance of a professional; delivered in a group setting and delivered on more than one occasion. No restrictions were placed on the type of comparator(s) or the type of outcomes captured in the study. We deliberately limited the study to professionally led activities to provide a sharper distinction between social events where arts and creativity may occur and arts and creativity interventions per se. We set no language restriction nor a restriction on the date from which studies were reported.
Search methods
PRESS (peer-review electronic search strategies) guidelines informed the design our search strategy [54, 55] and an information specialist adapted the search terms (outlined in Table S1) for the following electronic bibliographic databases: MEDLINE, PubMed, EMBASE, Econlit and Web of Science and NHSEED. We also inspected references of all relevant studies; and searched trials registers (ClinicalTrials.gov). Search terms used included cost, return on investment, economic, arts, music, storytelling, dancing, writing and older adult as well as social return on investment (SROI). The last search was performed on 09/11/2022. As many economic evaluations of ACIs (especially SROIs) are commissioned by government bodies or charitable organisations, a search of the grey literature was undertaken.
Handling searches
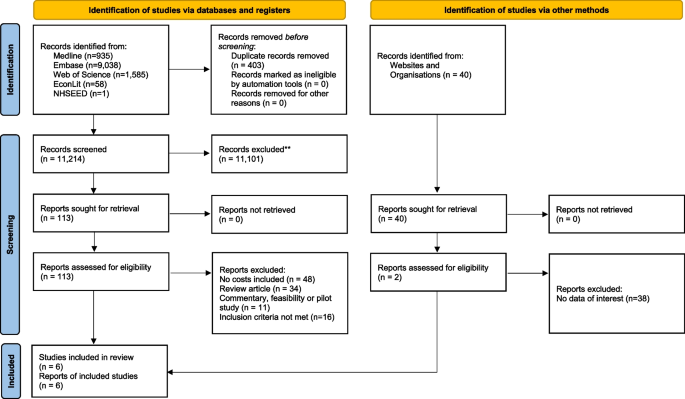
A PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow chart was used to document study selection, illustrating the numbers of records retrieved and selection flow through the screening rounds [56,57,58]; all excluded records (with rationale for exclusion) were documented.
Selection of studies
Two screening rounds were conducted independently by two health economists experienced in undertaking reviews (GC, CO’N). The first round screened the title and abstract of articles based on the eligibility criteria; those selected at this stage entered a second round of full text screening with eligibility based on the inclusion and exclusion criteria. Any disagreements were discussed among the two reviewers, with access to a third reviewer available to resolve disagreements, though this proved unnecessary.
Data extraction and management
Two reviewers extracted relevant information independently using an proforma developed specifically for the purposes of this study, which included all 35 items suggested by Wijnen et al. (2016) [48]. Information was extracted in relation to the following factors: (1) general information including study title, author, year, funding source, country, setting and study design; (2) recruitment details, sample size, demographic characteristics (age, gender) and baseline health data (diagnosis, comorbidities); (3) interventions, effectiveness and cost data; (4) type of economic evaluation, perspective, payer, beneficiary, time horizon, measure of benefit and scale of intervention; (5) quality assessment, strength of evidence, any other important information; (6) results; (7) analysis of uncertainty and (8) conclusions. The quality assessment/risk of bias checklists were included in the data extraction proforma, and picklists were used to enhance uniformity of responses. The data extraction form was piloted by two reviewers (GC and CON) on one paper and discussion used to ensure consistent application thereafter.
Assessment of study quality
Two reviewers (GC & CON) independently assessed study quality, with recourse to a third reviewer for resolution of differences though this proved unnecessary. Quality assessment was based on the type of economic evaluation undertaken. Full and partial trial-based economic evaluations were assessed using the CHEC-extended checklist [59]. SROI analyses were assessed using a SROI-specific quality framework developed for the purpose of systematic review [60].
Data analysis methods
Due to the small number of evaluations detected, possible sources of heterogeneity and a lack of consensus on appropriate methods for pooling cost-effectiveness estimates [61] a narrative synthesis analysis was undertaken.
Results
Database searches returned 11,619 records; from this, 402 duplicates were removed leaving 11,214 reports. From these 113 reports were assessment against the inclusion and exclusion criteria resulting in 4 studies for inclusion in the review. Over 40 websites were searched for relevant content returning 2 further studies for inclusion. The PRISMA 2020 diagram is presented in Fig. 1. A high sensitivity search strategy was adopted to ensure all relevant studies were identified, resulting in a large number of studies being excluded at the first stage of screening.
A total of six studies were identified; key characteristics are presented in Table 1. Identified studies were published between 2011 and 2020. Two studies used a health technology assessment (HTA) framework alongside clinical trials [62, 63] to assess the cost-effectiveness of community singing interventions. Both evaluations scored highly on the CHEC-extended checklist (Table 2), with findings reported in line with the CHEERS (Consolidated Health Economic Estimation Reporting Standards) checklist 2022 [64].
Four further studies employed an SROI framework to assess art and/or craft interventions: two studies were published in the peer-reviewed literature [65, 66] and a further two in the grey literature [67, 68]. All four adhered closely to the suggested steps for performing an SROI and consequently secured high scores (Table 3). No quality differential was discerned between those studies published in the academic literature when compared with those from the grey literature.
Five of the studies were undertaken in the UK [63, 66,67,68,69] and one in the US [63]. Four of the studies were designed for older adults with no cognitive impairment [62, 63, 67, 68]; one was designed for participants with or without dementia [65], and another was specifically for older adults with dementia and their caregivers [66]. Three of the studies were delivered in a community setting [62, 63, 67], two in care homes [65, 68] and one across a range of settings (hospital, community and residential) [66]. The length and duration of the ACIs varied; some lasted 1–2 h (with multiple classes available to participants) [65], whereas others were structured programmes with sessions lasting 90 min over a 14-week period [62]. The number of participants included in studies varied; the largest study contained data from 390 participants [63], whereas other studies measured engagement using numbers of care homes or housing associations included [67, 68].
Costs were captured from a narrower perspective (i.e., the payer—health service) for those economic evaluations which followed a health technology assessment (HTA) framework [62, 63]. Costs associated with providing the programme and health and social care utilisation costs were captured using cost diaries. Valuation of resource usage was in line with the reference case specified for each jurisdiction.
Social value analyses included in the review [65,66,67,68] captured a broader picture of cost; programme provision costs included were similar in nature to those identified using an HTA framework, however, the benefits captured went beyond the individual to capture costs to a wide range of stakeholders such as family members, activity co-ordinations and care home personnel. Costs were apportioned using financial proxies from a range of sources including HACT Social Value Bank [69] and market-based valuation methods.
The range of outcomes captured and valued across HTAs and SROIs was extensive: including, but not limited to, wellbeing, quality of life, physical health, cognitive functioning, communication, control over daily life choices, engagement and empowerment, social isolation, mobility, community inclusion, depressive symptoms, sadness, anxiety, loneliness, positive affect and interest in daily life. In the programmes assessed using an HTA framework, outcomes were captured using standardised and validated instruments, for both control and intervention groups across multiple time points. Statistical methods were used to assess changes in outcomes over time. Programmes assessed using SROI relied primarily on qualitative methods (such as reflective diaries and in-depth interviews) combined with routinely collected administrative data.
The evidence from the singing interventions was encouraging but not conclusive. The ‘Silver Song Club’ programme [62] reported a 64% probability of being cost-effective at a willingness-to-pay threshold of £30,000. This study was also included in the Public Health England (PHE) decision tool to support local commissioners in designing and implementing services to support older people’s healthy ageing, reporting a positive societal return on investment [70]. Evidence from the ‘Community of Voices’ trial [63] suggested that although intervention group members experienced statistically significant improvements in loneliness and interest in life compared to control participants, no significant group differences were observed for cognitive or physical outcomes or for healthcare costs.
A positive return on investment was reported by all social value analyses undertaken. The ‘Imagine Arts’ programme, reported a positive SROI of £1.20 for every £1 of expenditure [65]. A higher yield of between £3.20-£6.62 for each £1 invested was reported in the ‘Dementia and Imagination’ programme [66]. The ‘Craft Café’ programme, reported an SROI of £8.27 per £1 invested [68], and the ‘Creative Caring’ programme predicted a SROI of between £3 to £4 for every £1 spent [67]. The time period over which return on investment was calculated differed for each evaluation from less than one year to 4 years.
Discussion
The primary finding from our review concerns the paucity of evidence relating to the value, cost and/or cost-effectiveness of ACIs aimed at improving health and wellbeing in this population. Despite few restrictions being applied to our search, only six studies were found which met our inclusion criteria. This is not indicative of research into ACIs in this population, as evidenced by the identification of ninety-three studies where arts and creativity interventions were found to support better health and wellbeing outcomes in another recent review [5]. An alternative explanation is that funders do not see the added value of undertaking such evaluations in this area. That is, for funders, the cost of evaluating an ACIs is likely to be deemed unjustified given the relatively small welfare loss a misallocation of resources to them might produce. While at first glance this may seem reasonable, it disadvantages ACIs in competing with other interventions for funding and arguably exposes an implicit prejudice in the treatment of interventions from which it may be difficult to extract profit in general. That is, the paucity of evidence, may reflect inherent biases within our political economy that favour the generation of marketable solutions to health issues from which value can be appropriated as profit. Pharmaceuticals are an obvious example of such solutions, where the literature is replete with examples of evaluations sponsored by pharmaceutical companies or where public funds are used to test the claims made by pharmaceutical companies in respect of the value of their products. If the potential of ACIs to improve health and well-being is to be robustly established, ACIs must effectively compete for funding with other interventions including those from pharma. This requires a larger, more robust evidence base than is currently available and investment in the creation of such an evidence base. As there is currently no ‘for-profit’ industry to generate such an evidence base, public funding of evaluations will be central to its creation.
Our second finding concerns the values reported in the meagre evidence we did find. In five of the six studies we identified, evidence indicated that ACIs targeted at older people offered value for money [62, 65,66,67,68]. One study provided mixed evidence [63], however, in this study a ‘payer’ perspective was adopted when applying an HTA framework which, by virtue of the perspective adopted, excluded a range of benefits attributable to ACIs and public health interventions more generally. Among the four studies that adopted a SROI approach, estimated returns per £1 invested ranged from £1.20 to £8.27. Given the evident heterogeneity among studies in terms of context and methods, care is warranted in comparing estimates with each other or with other SROIs. Care is also required in accepting at face value the estimates reported given methodological issues that pertain to the current state of the art with respect to SROI. With these caveats in mind noted, the values reported for ACIs using the SROI approach are comparable with those from other SROI studies in other contexts including those as diverse as a first aid intervention [71], investment in urban greenways [72] and the provision of refuge services to those experiencing domestic violence [73] (a return on investment of £3.50-£4, £2.88-£5.81 and £4.94 respectively). Similarly, with respect to the study that adopted a cost-effectiveness approach, Coulton and colleagues (2015) reported a 64% probability of the intervention being cost-effective at a threshold of £30,000 [62]. Again, it is difficult to compare studies directly, but this is similar to that reported for interventions as diverse as a falls prevention initiative [74] and the treatment of depression using a collaborative approach [75] both in the UK. That the evidence base is meagre notwithstanding, there is, in other words, a prima facie case that ACIs are capable of offering value for money when targeted at older persons.
Our third finding relates to the state of the art with respect to SROIs in this area. Over the past 40 years, considerable time, effort and resources have been expended in the development of cost-effectiveness techniques in health and social care. While considerable heterogeneity can exist around their conduct, national guidance exists in many jurisdictions on the conduct of cost-effectiveness analyses (CEA) – such as the NICE reference case in the UK [76]– as well as in the reporting of these as set out in the CHEERS 2022 guidance [64]. This has helped raise the quality of published evaluations and the consistency with which they are reported. Despite the existence of a step-by-step guidance document on how to perform SROIs [77] which outlines how displacement effects, double counting, effect attribution and drop-off should be addressed, a significant body of work still remains to ensure that the methodology addresses a range of known biases in a robust manner. Where there is no comparator to the intervention being evaluated (as was the case in the SROIs reported here) it may be difficult to convince funders that the implicit incremental costs and benefits reported are indeed incremental and attributable to the intervention. Equally, where a comparator is present, greater consensus and standardisation is required regarding the identification, generation and application of, for example, financial proxies. Currently, SROI ratios combine value across a wide range of stakeholders, which is understandable if the objective is to capture all aspects of social benefit generated. This ratio, however, may not reflect the priorities and statutory responsibilities of healthcare funders. Whist all of the aforementioned issues can be addressed, investment is required to develop the SROI methodology further to more closely meet the needs of commissioning bodies.
Notwithstanding these challenges, social value analyses play a pivotal role within the procurement processes employed by government, local authorities and other non-departmental public bodies and should not be dismissed simply because the ‘burden of proof’ falls short of that required to secure remuneration within the health sector. As most SROIs are published in the grey literature, this means they often avoid peer scrutiny prior to publication and the potential quality assurance this can offer. It is noteworthy however that two of the SROIs included in this review [65, 66] were published in the academic literature, suggesting that the academic community are engaging with this method which is to be applauded.
Moving forward, it is unlikely we will be able to meet all of the health and wellbeing needs of our ageing population solely in a primary or secondary care setting. New models of care are required, as are new models of funding to support interventions which can be delivered in non-healthcare settings. New hybrid models of evaluation will be required to provide robust economic evidence to assist in the allocation of scarce resources across health and non-healthcare settings; such evaluative frameworks must have robust theoretical underpinnings and be capable of delivering evidence from a non-clinical setting in a timely and cost-effective manner.
In the absence of a definitive evaluation framework for ACIs being currently available, we have a number of recommendations. First, and most importantly, all impact assessments should have a control group or credible counterfactual. This is currently not required when performing an SROI making it difficult to determine if all of the benefits ascribed to an intervention are in fact attributable. This recommendation is in line with the conclusion of a report by the London School of Economics [78] for the National Audit Office (NAO) which concluded that ‘any impact evaluation (and subsequent value for money calculation) requires construction of a counterfactual’. Second, a detailed technical appendix should accompany all impact assessments to allow independent review by a subject specialist. While this would assist peer review, it would allow providing greater transparency where peer review was not undertaken prior to publication. Furthermore, it would enable recalculation of SROI ratios to exclude ‘value’ attributable to stakeholders which are not relevant to a particular funder. Third, equity considerations should be addressed explicitly in all evaluations (this is currently not required in HTAs). Fourth, both costs and outcomes should be captured from a ‘broad’ perspective (adopting a ‘narrow’ healthcare perspective may underestimate the full economic impact), with non-healthcare sector costs being detailed as part of the analysis. Finally, data should be collected post-implementation to ensure that resources continue to be allocated efficiently.
As with any review, there are limitations which should be noted. A search of the grey literature was included as evaluations of applied public health interventions are not always reported in the academic literature. Systematically identifying grey literature and grey data can be problematic [79,80,81,82,83] as it is not collected, organised or stored in a consistent manner. Hence it is possible that we have not identified all relevant studies. Furthermore, as applied public health interventions can be performed in a non-healthcare setting we included SROIs in our review of economic evaluations. Current guidance on the systematic review of economic evaluations has been developed primarily for review of HTA as opposed to public health interventions and hence SROIs would be excluded, or if included would score poorly due to the inherent biases arising from no comparator or counterfactual being included.
Conclusions
This systematic review found that participation in group-based arts and creativity programmes was generally cost-effective and/or produced a positive return on investment whilst having a positive impact on older people’s physical, psychological, and social health and wellbeing outcomes. Unfortunately, the small number of studies identified, coupled with differences in methods used to assess economic impact hinders our ability to conclusively determine which types of art and creativity-based activities are more cost-effective or represent best value for money.
As well as the need for a greater focus on prevention of poor health as we age, new hybrid models of healthcare delivery are necessary to meet the needs of our ageing population. These models will integrate traditional medical care with other services such as home health aides (some of which may include artificial intelligence), telemedicine and social support networks. Alongside these, ACIs have the potential to provide a low cost, scalable, easily implementable and cost-effective solution to reduce the burden of illness in this age group and support healthy ageing.
Evidence on the cost-effectiveness of a range of ACIs is of utmost importance for policy and decision makers as it can both inform the development of policies that support the provision of ACIs in the context of ageing, but also identify the most cost-effective approaches for delivering such interventions. The development of hybrid models of evaluation, capable of capturing cost-effectiveness and social value, is becoming increasingly necessary as healthcare delivery for this age group moves beyond the realms of primary and secondary care and into the community. The development and refinement of such models will ensure a more comprehensive assessment of the impact of a diverse range of interventions providing a more nuanced understanding of the impact of an intervention. This will help inform decision making and ensure interventions are implemented in a cost-effective and socially beneficial manner.
Availability of data and materials
All data generated or analysed during this study are included in the published article and its supplementary information files.
References
United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects: The 2015 Revision, Key Findings and Advance Tables. Working Paper No. ESA/P/WP.241. 2015.
Office for National Statistics. Living longer: how our population is changing and why it matters. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/ageing/articles/livinglongerhowourpopulationischangingandwhyitmatters/2018-08-13#how-do-incomes-of-older-people-compare-with-younger-ages. 2018. Accessed 07/12/2022
Dyakova M, Hamelmann C, Bellis MA, Besnier E, Grey CNB, Ashton K, Schwappach A, Clar C. Investment for health and well-being: a review of the social return on investment from public health policies to support implementing the Sustainable Development Goals by building on Health 2020 [Internet]. Copenhagen: WHO Regional Office for Europe; 2017.
Fancourt D, Finn S. What is the evidence on the role of the arts in improving health and well-being? A scoping review. Copenhagen: WHO Regional Office for Europe; 2019.
McQuade L, O’Sullivan R. Examining arts and creativity in later life and its impact on older people’s health and wellbeing: a systematic review of the evidence. Perspect Publ Health. 2023;0(0). https://doi.org/10.1177/17579139231157533
Skingley A, De’Ath S, Napleton L. Evaluation of Edna: arts and dance for older people. Work Older People. 2016;20(1):46–56.
Brustio PR, Liubicich ME, Chiabrero M, et al. Dancing in the golden age: a study on physical function, quality of life, and social engagement. Geriatr Nurs. 2018;39(6):635–9.
Beauchet O, Bastien T, Mittelman M, et al. Participatory art-based activity, community-dwelling older adults and changes in health condition: results from a pre-post intervention, single-arm, prospective and longitudinal study. Maturitas. 2020;134:8–14.
Roswiyani R, Hiew CH, Witteman CLM, et al. Art activities and qigong exercise for the well-being of older adults in nursing homes in Indonesia: a randomized controlled trial. Aging Ment Health. 2020;24(10):1569–78.
Shanahan J, Bhriain ON, Morris ME, et al. Irish set dancing classes for people with Parkinson’s disease: the needs of participants and dance teachers. Complement Ther Med. 2016;27:12–7.
Garcia Gouvêa JA, Antunes MD, Bortolozzi F, et al. Impact of senior dance on emotional and motor parameters and quality of life of the elderly. Rev Rene. 2017;18(1):51–8.
Sun J, Zhang N, Buys N, et al. The role of Tai Chi, cultural dancing, playing a musical instrument and singing in the prevention of chronic disease in Chinese older adults: a mind–body meditative approach. Int J Ment Health Pr. 2013;15:227–39.
Fu MC, Belza B, Nguyen H, et al. Impact of group-singing on older adult health in senior living communities: a pilot study. Arch Gerontol Geriatr. 2018;76:138–46.
Feng L, Romero-Garcia R, Suckling J, et al. Effects of choral singing versus health education on cognitive decline and aging: a randomized controlled trial. Aging-us. 2020;12(24):24798–816.
Seinfeld S, Figueroa H, Ortiz-Gil J, et al. Effects of music learning and piano practice on cognitive function, mood and quality of life in older adults. Front Psychol. 2013;4:810.
MacRitchie J, Breaden M, Milne AJ, et al. Cognitive, motor and social factors of music instrument training programs for older adults’ improved wellbeing. Front Psychol. 2020;10:2868.
Freeman WJI. A neurobiological role of music in social bonding. In: Wallin N, Merkur B, Brown S, editors. The origins of music. Cambridge: MIT Press; 2000. http://escholarship.org/uc/item/9025x8rt.
Huron D. Is music an evolutionary adaptation? Ann N Y Acad Sci. 2001;930(1):43–61. https://doi.org/10.1111/j.1749-6632.2001.tb05724.x.
Tarr B, Launay J, Dunbar RIM. Music and social bonding: “self–other” merging and neurohormonal mechanisms. Front Psychol. 2014;5:1096. https://doi.org/10.3389/fpsyg.2014.01096.
Cain M, Lakhani A, Istvandity L. Short and long term outcomes for culturally and linguistically diverse (cald) and at-risk communities in participatory music programs: a systematic review. Arts Health. 2016;8(2):105–24. https://doi.org/10.1080/17533015.2015.1027934.
Martin L, Oepen R, Bauer K, Nottensteiner A, Mergheim K, Gruber H, et al. Creative arts interventions for stress management and prevention – a systematic review. Behav Sci (Basel). 2018;8(2):pii:E28. https://doi.org/10.3390/bs8020028.
Linnemann A, Wenzel M, Grammes J, Kubiak T, Nater UM. Music listening and stress in daily life: a matter of timing. Int J Behav Med. 2018;25(2):223–30. https://doi.org/10.1007/s12529-017-9697-5.
Linnemann A, Strahler J, Nater UM. The stress-reducing effect of music listening varies depending on the social context. Psychoneuroendocrinology. 2016;72:97–105. https://doi.org/10.1016/j.psyneuen.2016.06.003.
Panteleeva Y, Ceschi G, Glowinski D, Courvoisier DS, Grandjean DM. Music for anxiety? meta-analysis of anxiety reduction in non-clinical samples. Psychol Music. 2017;46(4):473–87. https://doi.org/10.1177/0305735617712424.
Fancourt D, Tymoszuk U. Cultural engagement and incident depression in older adults: evidence from the English longitudinal study of ageing. Br J Psychiatry. 2018;214(4):225–9. https://doi.org/10.1192/bjp.2018.267.
Balbag MA, Pedersen NL, Gatz M. Playing a musical instrument as a protective factor against dementia and cognitive impairment: a population-based twin study. Int J Alzheimer’s Dis. 2014;2014:836748. https://doi.org/10.1155/2014/836748.
Porat S, Goukasian N, Hwang KS, Zanto T, Do T, Pierce J, et al. Dance experience and associations with cortical gray matter thickness in the aging population. Dement Geriatr Cogn Dis Extra. 2016;6(3):508–17. https://doi.org/10.1159/000449130.
Federici A, Bellagamba S, Rocchi MBL. Does dance-based training improve balance in adult and young old subjects? a pilot randomized controlled trial. Aging Clin Exp Res. 2005;17(5):385–9 PMID: 16392413.
Alpert PT, Miller SK, Wallmann H, Havey R, Cross C, Chevalia T, et al. The effect of modified jazz dance on balance, cognition, and mood in older adults. J Am Acad Nurse Pract. 2009;21(2):108–15. https://doi.org/10.1111/j.1745-7599.2008.00392.x.
Jeon MY, Bark ES, Lee EG, Im JS, Jeong BS, Choe ES. The effects of a Korean traditional dance movement program in elderly women. Taehan Kanho Hakhoe Chi. 2005;35(7):126876 (in Korean). PMID: 16418553.
Eyigor S, Karapolat H, Durmaz B, Ibisoglu U, Cakir S. A randomized controlled trial of Turkish folklore dance on the physical performance, balance, depression and quality of life in older women. Arch Gerontol Geriatr. 2009;48(1):84–8. https://doi.org/10.1016/j.archger.2007.10.008.
Noopud P, Suputtitada A, Khongprasert S, Kanungsukkasem V. Effects of Thai traditional dance on balance performance in daily life among older women. Aging Clin Exp Res. 2018;31(7):961–7. https://doi.org/10.1007/s40520-018-1040-8.
Trombetti A, Hars M, Herrmann FR, Kressig RW, Ferrari S, Rizzoli R. Effect of musicbased multitask training on gait, balance, and fall risk in elderly people: a randomized controlled trial. Arch Intern Med. 2011;171(6):525–33. https://doi.org/10.1001/archinternmed.2010.446.
Hyyppä MT, Mäki J, Impivaara O, Aromaa A. Individual-level measures of social capital as predictors of all-cause and cardiovascular mortality: a population-based prospective study of men and women in Finland. Eur J Epidemiol. 2007;22(9):589–97. https://doi.org/10.1007/s10654-007-9153-y.
Hyyppä MT, Mäki J, Impivaara O, Aromaa A. Leisure participation predicts survival: a population-based study in Finland. Health Promot Int. 2006;21(1):5–12. https://doi.org/10.1093/heapro/dai027.
Lennartsson C, Silverstein M. Does engagement with life enhance survival of elderly people in Sweden? the role of social and leisure activities. J Gerontol B Psychol Sci Soc Sci. 2001;56(6):S335–42. https://doi.org/10.1093/geronb/56.6.s335.
Sundquist K, Lindström M, Malmström M, Johansson SE, Sundquist J. Social participation and coronary heart disease: a follow-up study of 6900 women and men in Sweden. Soc Sci Med. 1982;58(3):615–22. https://doi.org/10.1016/s0277-9536(03)00229-6.
Väänänen A, Murray M, Koskinen A, Vahtera J, Kouvonen A, Kivimäki M. Engagement in cultural activities and cause-specific mortality: prospective cohort study. Prev Med. 2009;49(2–3):142–7. https://doi.org/10.1016/j.ypmed.2009.06.026.
Särkämö T, Soto D. Music listening after stroke: beneficial effects and potential neural mechanisms. Ann N Y Acad Sci. 2012;1252(1):266–81. https://doi.org/10.1111/j.1749-6632.2011.06405.x.
Särkämö T, Pihko E, Laitinen S, Forsblom A, Soinila S, Mikkonen M, et al. Music and speech listening enhance the recovery of early sensory processing after stroke. J Cogn Neurosci. 2010;22(12):2716–27. https://doi.org/10.1162/jocn.2009.21376.
Särkämö T, Ripollés P, Vepsäläinen H, Autti T, Silvenno HM, Salli E, et al. Structural changes induced by daily music listening in the recovering brain after middle cerebral artery stroke: a voxel-based morphometry study. Front Hum Neurosci. 2014;8:245. https://doi.org/10.3389/fnhum.2014.00245.
Särkämö T, Tervaniemi M, Laitinen S, Forsblom A, Soinila S, Mikkonen M, et al. Music listening enhances cognitive recovery and mood after middle cerebral artery stroke. Brain. 2008;131(3):866–76. https://doi.org/10.1093/brain/awn013.
Fancourt D, Steptoe A, Cadar D. Cultural engagement and cognitive reserve: museum attendance and dementia incidence over a 10-year period. Br J Psychiatry. 2018;213(5):661–3. https://doi.org/10.1192/bjp.2018.129.
Fancourt D, Steptoe A, Cadar D. Cultural engagement predicts changes in cognitive function in older adults over a 10 year period: findings from the English longitudinal study of ageing. Sci Rep. 2018;8(1):10226. https://doi.org/10.1192/bjp.2018.129.
All Party Parliamentary group on arts, health and wellbeing. Creative health: the arts for health and wellbeing. 2017.
van Mastrigt GA, Hiligsmann M, Arts JJ, Broos PH, Kleijnen J, Evers SM, Majoie MH. How to prepare a systematic review of economic evaluations for informing evidence-based healthcare decisions: a five-step approach (part 1/3). Expert Rev Pharmacoecon Outcomes Res. 2016;16(6):689–704. https://doi.org/10.1080/14737167.2016.1246960. Epub 2016 Nov 2 PMID: 27805469.
Thielen FW, Van Mastrigt G, Burgers LT, Bramer WM, Majoie H, Evers S, Kleijnen J. How to prepare a systematic review of economic evaluations for clinical practice guidelines: database selection and search strategy development (part 2/3). Expert Rev Pharmacoecon Outcomes Res. 2016;16(6):705–21. https://doi.org/10.1080/14737167.2016.1246962. Epub 2016 Nov 2 PMID: 27805466.
Wijnen B, Van Mastrigt G, Redekop WK, Majoie H, De Kinderen R, Evers S. How to prepare a systematic review of economic evaluations for informing evidence-based healthcare decisions: data extraction, risk of bias, and transferability (part 3/3). Expert Rev Pharmacoecon Outcomes Res. 2016;16(6):723–32. https://doi.org/10.1080/14737167.2016.1246961. Epub 2016 Oct 21 PMID: 27762640.
Mandrik OL, Severens JLH, Bardach A, Ghabri S, Hamel C, Mathes T, Vale L, Wisløff T, Goldhaber-Fiebert JD. Critical appraisal of systematic reviews with costs and cost-effectiveness outcomes: an ISPOR good practices task force report. Value Health. 2021;24(4):463–72. https://doi.org/10.1016/j.jval.2021.01.002. PMID: 33840423.
Kelly MP, McDaid D, Ludbrook A, Powell J: Economic appraisal of public health interventions. http://www.cawt.com/Site/11/Documents/Publications/Population%20Health/Economics%20of%20Health%20Improvement/Economic_appraisal_of_public_health_interventions.pdf
Weatherly H, Drummond M, Claxton K, Cookson R, Ferguson B, Godfrey C, Rice N, Sculpher M, Sowden A. Methods for assessing the cost-effectiveness of public health interventions: key challenges and recommendations. Health Policy. 2009;93(2–3):85–92. https://doi.org/10.1016/j.healthpol.2009.07.012. Epub 2009 Aug 25 PMID: 19709773.
Payne K, McAllister M, Davies LM. Valuing the economic benefits of complex interventions: when maximising health is not sufficient. Health Econ. 2012. https://doi.org/10.1002/hec.2795.
Edwards RT, Charles JM, Lloyd-Williams H. Public health economics: a systematic review of guidance for the economic evaluation of public health interventions and discussion of key methodological issues. BMC Public Health. 2013;24(13):1001. https://doi.org/10.1186/1471-2458-13-1001.PMID:24153037;PMCID:PMC4015185.
Rethlefsen ML, Farrell AM, Osterhaus Trzasko LC, Brigham TJ. Librarian co-authors correlated with higher quality reported search strategies in general internal medicine systematic reviews. J Clin Epidemiol. 2015;68(6):617–26. https://doi.org/10.1016/j.jclinepi.2014.11.025. Epub 2015 Feb 7 PMID: 25766056.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6. https://doi.org/10.1016/j.jclinepi.2016.01.021. Epub 2016 Mar 19 PMID: 27005575.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med. 2008;6:e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;21(339):b2700. https://doi.org/10.1136/bmj.b2700.PMID:19622552;PMCID:PMC2714672.
Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. PLoS Med. 2009;6(7):e1000097 Evers S, Goossens M, De Vet H, et al. Criteria list for assessment of methodological quality of economic evaluations: consensus on health economic criteria. Int J Technol Assess Health Care. 2005;21(02):240–245.
Evers S, Goossens M, de Vet H, van Tulder M, Ament A. Criteria list for assessment of methodological quality of economic evaluations: Consensus on Health Economic Criteria. Int J Technol Assess Health Care. 2005;21(2):240–5 PMID: 15921065.
Hutchinson CL, Berndt A, Gilbert-Hunt S, George S, Ratcliffe J. Valuing the impact of health and social care programmes using social return on investment analysis: how have academics advanced the methodology? A protocol for a systematic review of peer-reviewed literature. BMJ Open. 2018;8(12):e022534. https://doi.org/10.1136/bmjopen-2018-022534. PMID:30530579;PMCID:PMC6303612.
Higgins J, Green S. Cochrane handbook for systematic reviews of interventions version 5.1. 0. Chichester: The Cochrane Collaboration; 2013.
Coulton S, Clift S, Skingley A, Rodriguez J. Effectiveness and cost-effectiveness of community singing on mental health-related quality of life of older people: randomised controlled trial. Br J Psychiatry. 2015;207(3):250–5. https://doi.org/10.1192/bjp.bp.113.129908. Epub 2015 Jun 18 PMID: 26089304.
Johnson JK, Stewart AL, Acree M, Nápoles AM, Flatt JD, Max WB, Gregorich SE. A community choir intervention to promote well-being among diverse older adults: results from the community of voices trial. J Gerontol B Psychol Sci Soc Sci. 2020;75(3):549–59. https://doi.org/10.1093/geronb/gby132. PMID:30412233;PMCID:PMC7328053.
Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, Caulley L, Chaiyakunapruk N, Greenberg D, Loder E, Mauskopf J, Mullins CD, Petrou S, Pwu RF, Staniszewska S, CHEERS 2022 ISPOR Good Research Practices Task Force. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Value Health. 2022;25(1):3–9. https://doi.org/10.1016/j.jval.2021.11.1351. PMID: 35031096.
Bosco A, Schneider J, Broome E. The social value of the arts for care home residents in England: a social return on investment (SROI) analysis of the imagine arts programme. Maturitas. 2019;124:15–24. https://doi.org/10.1016/j.maturitas.2019.02.005. Epub 2019 Mar 13 PMID: 31097173.
Jones C, Windle G, Edwards RT. Dementia and imagination: a social return on investment analysis framework for art activities for people living with dementia. Gerontologist. 2020;60(1):112–23. https://doi.org/10.1093/geront/gny147. PMID: 30476114.
Social Value Lab and Impact Arts Craft Café: creative solutions to isolation and loneliness; Social return on investment. 2011. http://www.socialvaluelab.org.uk/wp-content/uploads/2013/05/CraftCafeSROI.pdf
MB associates. Make my day: the impact of Creative Caring in older people’s care homes. 2013. https://www.suffolkartlink.org.uk/wp-content/uploads/2014/10/CreativeCarersSROIReport_Nov2013.pdf
HACT. n.d. UK Social Value Bank. Retrieved December 11, 2023. from https://hact.org.uk/tools-and-services/uk-social-value-bank/.
The Older Adults’ NHS and social care return on investment tool. Project report. Public health England. December 2019. Last accessed 27/03/2023.
British Red Cross – Valuing First Aid Education. 2018. https://socialvalueuk.org/wp-content/uploads/2018/12/Valuing-First-Aid-Education-Social-Return-on-Investment-Report-on-the-value-of-First-Aid-Education-Assured-Report.pdf. Accessed 17/02/2023
Hunter R, Dallat M, Tully M, O’Neill C, Heron L, Kee F. Social return on investment analysis of an urban greenway. Cities and Health. 2020. https://doi.org/10.1080/23748834.2020.1766783.
NEF Consulting. Refuge: A social return on investment evaluation. 2016. https://socialvalueuk.org/wp-content/uploads/2017/04/Refuge-SROI-2016.pdf Accessed 17/02/2022
Corbacho B, Cockayne S, Fairhurst C, Hewitt CE, Hicks K, Kenan AM, Lamb SE, MacIntosh C, Menz HB, Redmond AC, Rodgers S, Scantlebury A, Watson J, Torgerson DJ, on behalf of the REFORM study. Cost-Effectiveness of a Multifaceted Podiatry Intervention for the Prevention of Falls in Older People: The REducing Falls with Orthoses and a Multifaceted Podiatry Intervention Trial Findings. Gerontology. 2018;64(5):503–12. https://doi.org/10.1159/000489171. Epub 2018 Jun 26 PMID: 29945150.
Green C, Richards DA, Hill JJ, Gask L, Lovell K, Chew-Graham C, Bower P, Cape J, Pilling S, Araya R, Kessler D, Bland JM, Gilbody S, Lewis G, Manning C, Hughes-Morley A, Barkham M. Cost-effectiveness of collaborative care for depression in UK primary care: economic evaluation of a randomised controlled trial (CADET). PLoS ONE. 2014;9(8):e104225. https://doi.org/10.1371/journal.pone.0104225.PMID:25121991;PMCID:PMC4133193.
National Institute for Health and Care Excellence (NICE). NICE health technology evaluations: the manual. 2022. Retrieved 27 March, 2023 from https://www.nice.org.uk/process/pmg36/chapter/introduction-to-health-technology-evaluation
NEF Consulting. SSE – Beatrice SROI framework – guidance document. https://www.sse.com/media/svnn5jpk/sroi-methodology-guidance-nef-consulting.pdf. Accessed 17/02/2022
Gibbons S, McNally S, Overman H. Review of Government Evaluations: A report for the NAO. London: National Audit Office; 2013.
Turner AM, Liddy ED, Bradley J, Wheatley JA. Modeling public health interventions for improved access to the gray literature. J Med Libr Assoc. 2005;93(4):487–94 PMID: 16239945; PMCID: PMC1250325.
Benzies KM, Premji S, Hayden KA, Serrett K. State-of-the-evidence reviews: advantages and challenges of including grey literature. Worldviews Evid Based Nurs. 2006;3(2):55–61. https://doi.org/10.1111/j.1741-6787.2006.00051.x. PMID: 17040510.
Franks H, Hardiker NR, McGrath M, McQuarrie C. Public health interventions and behaviour change: reviewing the grey literature. Public Health. 2012;126(1):12–7. https://doi.org/10.1016/j.puhe.2011.09.023. Epub 2011 Nov 29 PMID: 22130477.
Mahood Q, Van Eerd D, Irvin E. Searching for grey literature for systematic reviews: challenges and benefits. Res Synth Methods. 2014;5(3):221–34. https://doi.org/10.1002/jrsm.1106. Epub 2013 Dec 6 PMID: 26052848.
Godin K, Stapleton J, Kirkpatrick SI, Hanning RM, Leatherdale ST. Applying systematic review search methods to the grey literature: a case study examining guidelines for school-based breakfast programs in Canada. Syst Rev. 2015;22(4):138. https://doi.org/10.1186/s13643-015-0125-0. PMID:26494010;PMCID:PMC4619264.
Acknowledgements
We would like to thank Ms. Louise Bradley (Information Resource Officer, Institute of Public Health) for her assistance in refining search strategies and literature search.
Funding
This study was supported by the Institute of Public Health (IPH), 200 South Circular Road, Dublin 8, Ireland, D08 NH90. This study was a collaboration between two health economists (GC, CO’N) and two members of staff from the funding organisation (LM, RO’S). Input from IPH staff was fundamental in defining the scope of work and research question, refining search terms and review and editing of the manuscript. Staff from IPH were not involved in quality assurance or review of papers included in the manuscript.
Author information
Authors and Affiliations
Contributions
LMcQ and ROS were involved in defining the scope of work, refining the research question, provision of subject specific (public health) context, review of search strategy, review & editing of manuscript. CON and GC were involved in refining the research question and search strategy, provision of health economics and systematic reviewing expertise, review of returned reports, original draft preparation, review, editing and submission of manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table S1. Search strategy for electronic databases and grey literature.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Crealey, G., McQuade, L., O’Sullivan, R. et al. Arts and creativity interventions for improving health and wellbeing in older adults: a systematic literature review of economic evaluation studies. BMC Public Health 23, 2496 (2023). https://doi.org/10.1186/s12889-023-17369-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17369-x