- Study Protocol
- Open access
- Published:
Multicentre case–control study of pneumococcal infections among children with pneumonia in Peninsular Malaysia (MY-Pneumo): a study protocol
BMC Public Health volume 24, Article number: 2255 (2024)
Abstract
Background
S. pneumoniae (SPN) is the most common cause of pneumonia. The disease can be effectively prevented through immunisation. Since December 2020, the Malaysian Government has included the 10-valent pneumococcal conjugate vaccine (PCV10) for all infants born on or after 1 January 2020 as part of the National Immunisation Programme (NIP). However, the epidemiology of pneumonia remains poorly understood. To fill the knowledge gap, we established a multicentre surveillance study to understand the burden of pneumococcal pneumonia among young children in Peninsular Malaysia.
Methods
MY-Pneumo is a multicentre prospective case–control study conducted in three sentinel sites located in three different states of Peninsular Malaysia – Kuala Lumpur, Pahang, and Kelantan. A cohort of at least 500 incident cases and 500 controls is enrolled beginning in October 2021 and matched for age. Cases are hospitalised children < 5 years with radiologically confirmed pneumonia, and the controls are children without any features suggestive of pneumonia. Clinical samples, including nasopharyngeal swabs (NPS) and urine, are collected according to the study protocol. Biological fluids such as blood, cerebrospinal fluid (CSF) and pleural fluid are obtained from invasive pneumonia disease (IPD) patients, if available. All children are tested for SPN using polymerase chain reaction (PCR) and pneumococcal urine antigen test (PUAT) using BinaxNow.
Discussion
Surveillance data, including carriage rate, serotype variations and the phylogeny data structure of SPN among young children in Malaysia during PCV implementation, will be generated from this study. Trends and patterns of pneumococcal serotypes by different regions are important for targeted public health strategies. Our data will provide baseline information for estimating the impact of PCV10 implementation and will influence policymakers' decisions regarding the upgrade from PCV10 to a higher-valency conjugate vaccine in Malaysia.
Trial registration
This project was registered at ClinicalTrials.gov (NCT04923035) on 2021, June 11. The study protocol was approved by the International Medical University Joint-Committee on Research & Ethics (4.15/JCM-216/2021) and the Institutional Review Board at sentinel sites (USM/JEPeM/21020190, IREC 2021–114, MREC ID No: 2021128–9769) and University of Southampton's Ethics and Research Governance (ERGo II 64844).
Background
According to the World Health Organization (WHO), pneumonia accounts for a substantial portion of deaths in children under five [1]. The burden of pneumonia is high in developing countries with limited access to healthcare resources, overcrowding and vaccines. Preventive measures, such as routine vaccinations, exclusive breastfeeding, good nutrition, and reducing exposure to indoor air pollution, can reduce the risk of pneumonia in children [2,3,4]. Additionally, timely diagnosis and appropriate treatment, including the use of antibiotics when necessary, are crucial in managing pneumonia and preventing severe outcomes [5, 6].
The most common cause of pneumonia among children under five is infection with Streptococcus pneumoniae (SPN), also known as pneumococcus. Immunisation with a pneumococcal vaccine is an effective way to prevent pneumonia. In Malaysia, pneumococcal vaccination under the NIP for children has commenced for infants born from January 2020, comprising three doses at 4, 6 and 15 months. The routine use of the 10-valent pneumococcal conjugate vaccine (PCV10) in children is expected to reduce the burden of pneumococcal infections in the country, especially severe infections. The impact of the coronavirus disease 2019 (COVID-19) pandemic may also have implications on the pneumococcal serotype and clinical presentation of infections in the community. There was a 30% to 80% decline in IPD incidence rate observed for all pneumococcal serotype groups in England and the Netherlands populations, respectively [7, 8]. In Malaysia, children with severe pneumonia due to COVID-19 exhibited a less severe clinical trajectory when compared with cases caused by other respiratory viruses [9]. The children manifested early in the disease progression, exhibiting no atypical biomarkers, such as lymphopenia and elevated C-reactive protein (CRP) levels. There were no invasive pneumococcal coinfections despite the low pneumococcal vaccination rates among the study population [9]. Therefore, we conducted a prospective case–control study to understand the burden of pneumococcal pneumonia in young children and to provide a baseline assessment to monitor changes in SPN carriage post-PCV implementation in Malaysia.
Methods/design
Study objectives
The study’s primary objectives are to provide baseline surveillance of pneumococcal pneumonia in young children in Malaysia by determining the prevalence of SPN nasopharyngeal carriage among children aged 5 years and below with pneumonia and IPD. Secondary study objectives are: 1) to determine SPN serotypes by polymerase chain reaction (PCR) and whole-genome sequencing (WGS), 2) to evaluate the correlation of SPN detection between nasopharyngeal carriage and urine samples, and 3) to establish sensitivity and specificity cutoffs of BinaxNOW for the detection of SPN serotypes in children with pneumonia and IPD.
Study size power calculation
This is a prospective case–control study in which all children aged 5 years and below with clinically diagnosed pneumonia and healthy controls will be recruited at three study sites. As per assumptions of 95% confidence interval (CI), 80% power and detectable odds ratio (OR) of 1.5, we estimate 164 cases and 164 healthy controls per sentinel hospital site. Thus, we aim to recruit a total of 500 confirmed pneumonia/IPD cases and 500 healthy controls for this study.
Study sites and design
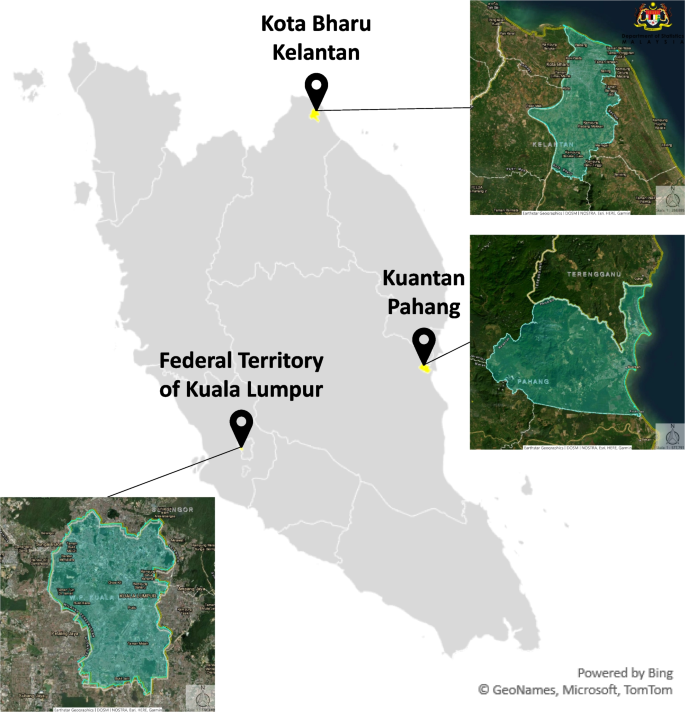
This prospective, hospital-based, multicentre case–control study is being conducted at three university hospitals in different states within Peninsular Malaysia – Kuala Lumpur, Pahang, and Kelantan (Fig. 1). Kuala Lumpur serves as the capital city of Malaysia and is centrally located in the western part of Peninsular Malaysia. Pahang and Kelantan are located on the east coast of Peninsular Malaysia, along the South China Sea, providing them with access to the coastline. Kelantan is situated to the north of Kuantan and shares its eastern border with Thailand. Study enrolment is at 1) University Malaya Medical Centre (UMMC), Kuala Lumpur; 2) Hospital Universiti Sains Malaysia (HUSM), Kota Bharu, Kelantan; and 3) Sultan Ahmad Shah Medical Centre International Islamic University Malaysia (SASMEC IIUM), Kuantan, Pahang. Table 1 summarises the demographics and burden of pneumonia in each state of the participating sentinel site. Cases and controls are age-matched within the range of 6 months. Cases are age-matched children clinically diagnosed with pneumonia and attending the outpatient department or admitted as a hospital inpatient, Invasive Pneumococcal Disease (IPD) (without pneumonia), bacteraemic pneumococcal pneumonia, and chest radiograph (CXR) confirmed pneumonia (by WHO guideline) [10]. Controls are healthy age-matched children without any intercurrent respiratory illness. Subject enrollment is over 24 months for each participating site, and a total sample of 400 subjects (200 cases and 200 controls) is targeted for UMMC and HUSM, respectively, and 200 subjects (100 cases and 100 controls) for IIUM. Male and female patients from the three major ethnic groups (Malay, Chinese, and Indian) are being recruited from each sentinel site. The study protocol workflow is as outlined in Fig. 2.
Geographical locations of participating university hospitals in Peninsular Malaysia: Kuala Lumpur, Pahang, and Kelantan. Source: Adapted from Department of Statistics, Malaysia. (2023, August 16). https://statsgeo.mycensus.gov.my/geostats/report.php
Summary of the study protocol workflow. The specimen collection, processing, and storage of nasopharyngeal swabs (NPS) were adapted from CDC Pneumococcal Carriage Protocols. Clinical samples were taken according to local policy, including NPS and urine samples. Different methods were used to collect the urine depending on the age and tolerability of the participant i.e. clean catch/void, urine collection bag, and diaper. Additional blood, cerebrospinal fluid (CSF) and pleural fluid were taken for invasive pneumococcal disease (IPD) patients, if available. NPS was inoculated into a medium containing skim milk, tryptone, glucose, and glycerin (STGG) and stored at -80 °C before shipment to IMU-Advanced Microbiology Collaborative Research Laboratory (AMCRL). General questionnaires/case report form (CRF) were administered to the parents/caregivers of the patients to obtain socio-demographic, vaccination history and medical history of the child. The gene targets for pneumococcal identification, including the main pneumococcal capsular biosynthesis gene A (cpsA), were analysed through PCR. SPN isolates will be transferred to the University of Southampton (UoS), United Kingdom (UK), for whole-genome sequencing (WGS) analysis
Study participants
The study population is comprised of children under 5 years of age who comply with protocol definitions and inclusion criteria. Eligible participants are identified by study paediatricians and research assistants at each participating site. The following criteria define cases: 1) hospitalised patients aged between 2 weeks and 59 months, 2) clinical features of pneumonia, as described below, 3) radiological confirmation of pneumonia based on CXR findings as per WHO guidelines [10], and 4) an informed consent statement signed by the children’s parents or legal guardian. The exclusion criteria for cases are the following: children who 1) do not meet the case definition, and 2) whose parents or legal guardian declined to sign the informed consent statement. Controls are defined by children aged 5 years and below, who are in good health, as determined by a brief medical history and/or clinical judgement of the investigator, and whose parent or legal guardian is willing and able to give informed consent. Exclusion criteria for the controls are: 1) any symptom suggestive of respiratory illness, 2) has nasal surgery, 3) has significant diseases or symptoms, such as febrile illness or a temperature ≥ 38 °C on the day of the visit or in the preceding 72 h that can place the patient at an increased risk of the disease, 4) has a history of antibiotic administration in the month prior to sampling, or 5) minors whose parents or legal guardian decline to sign the informed consent statement. Cases and controls are matched for study site and age (± 6 months). General questionnaires are administered to the parents or legal guardians of the participants to obtain demographic and socio-economic data and their medical history. Subjects are identified based on an anonymised identifier. The master list is kept in a password-protected spreadsheet.
Definition of pneumonia
Pneumonia cases are defined as patients with a history of cough and/or difficulty/rapid breathing and/or intercostal recession, with or without fever, and radiological confirmation of pneumonia as per WHO guidelines [10].
Biological samples
Samples are collected in the first 24 h of patient hospitalisation (Table 2). Nasopharyngeal swabs (NPS) and urine samples are collected from all pneumonia cases and controls following Centers for Disease Control and Prevention (CDC) Pneumococcal Carriage Protocols [11]. Each sample is aliquoted as per protocols outlined in this study. Each NPS is inoculated into a medium containing skim milk, tryptone, glucose, and glycerol (STGG) and stored at -80 °C before shipment to the International Medical University Advanced Microbiology Collaborative Research Laboratory (IMU-AMCRL) in Kuala Lumpur, Malaysia, every 4 months by a licensed/registered courier. One NPS and one 15 mL urine sample are collected from each subject at the time of enrolment. The collection procedure is performed by trained clinical staff, nurses, and the research assistant at the sentinel site. The NPS collection procedure involves inserting a nylon-tipped FLOQswab (COPAN Diagnostics Inc., USA) through the nostril into the cavity between the nose and mouth for 5 s and rotating it several times. The swab is then inserted into a cryovial with 1 mL of STGG media (2% (w/v) skim milk powder, 3% (w/v) tryptone soy broth powder, 0.5% (w/v) glucose and 10% (v/v) glycerol in water), and immediately vortexed briefly and frozen at -80 °C within 4 h. Different methods of urine collection are used depending on the age and tolerability of the participant, such as clean catch or void, urine collection bag, and diaper. Briefly, for children using diapers, we used the “urine ball method”, which involves placing sterile cotton balls on the subject’s diaper. The urine is subsequently collected by placing the urine-soaked cotton balls into a sterile 20 mL syringe, and the fluid is extracted with a plunger. The collected urine is mixed with PIPES buffer and aliquoted into three tubes of 5 ml each. All urine sampling supplies, including tubes, urine bags, buffer and BinaxNOW test kits, are provided to sentinel sites by Merck Sharp & Dohme (MSD) via Pharmaceutical Product Development (PPD). Urine samples are tested with BinaxNOW at sentinel sites, and the remaining aliquots are shipped to the MSD Central Lab on dry ice. The BinaxNOW® test kit includes a test device (strip or card), a specimen swab, and a buffer solution. The test device is placed on a clean, flat surface before a buffer solution is added from a dropper bottle. A specimen swab is dipped into the urine specimen, removed, and then inserted into the test card. The card is then closed, bringing the specimen into contact with the test strip. Pneumococcal antigen present in the specimen reacts to bind anti-S. pneumoniae-conjugated antibody. The resulting antigen-conjugate complexes are captured by immobilised anti-S. pneumoniae antibody, forming the Sample Line. Immobilised control antibody captures anti-species conjugate, forming the Control Line. Test results are interpreted by the presence or absence of visually detectable pink-to-purple coloured lines. A positive test result, read in 15 min, will include the detection of both a Sample and a Control Line. A negative test result, read in 15 min, will produce only a Control Line, indicating that S. pneumoniae antigen was not detected in the specimen. Failure of the Control Line to appear, whether the Sample Line is present or not, indicates an invalid assay. Additional blood, cerebrospinal fluid (CSF) and pleural fluid will be taken for IPD patients, if available, at each sentinel hospital site.
Laboratory analysis
Laboratory isolation (including genomic deoxyribonucleic acid (DNA) extraction), identification and confirmation of SPN in each sample are carried out at the IMU-AMCRL. Aliquots of NPS in STGG media include volumes of 400 µl, 350 µl and 250 µl, are stored in -80 °C freezers. The 250 µl NPS-STGG aliquot is the working sample used for blood agar culture, optochin-sensitivity, and DNA extraction for each participant. A 10 µl loopful of sample is taken from the 250 µl aliquot, plated onto Columbia agar with 5% sheep blood (CBA) (Oxoid), and incubated in 5% CO2 at 37 °C for 24 h. The plate culture is observed after 24 h of incubation, and colonies exhibiting SPN morphology are picked for replating onto fresh CBA plates with 5 mcg optochin disc (HIMEDIA), followed by incubation as in the previous step. SPN isolates are identified as small, greyish, alpha-hemolytic culture growths showing Draughtsman morphology, and are optochin sensitive. Genomic DNA from the remaining 240 µl NPS-STGG aliquot is extracted using the New England Biolabs (NEB) Monarch® Genomic DNA Purification Kit (USA). The extracted genomic DNA is then subjected to multiplex conventional PCR analysis according to the CDC protocol (US scheme protocol) to detect SPN serotypes by amplifying the capsular polysaccharide biosynthesis gene A (cpsA) targets. SPN isolates will be transferred to the University of Southampton (UoS), United Kingdom (UK), for WGS analysis. Isolates will be sequenced using a MiSeq (Illumina, UK) to generate 2 × 300 paired-end data. Assembly will be done using SPAdes with assembly improvement and QC as described previously [12].
Data sources and quality control
Clinical site monitoring for research conduct and management is conducted yearly by the Principal Investigator team from the International Medical University (IMU). The main purpose of clinical site monitoring is primarily to ensure protocol adherence, source data verification, investigator training, site performance, data quality assurance, and maintaining data integrity at each participating site. Tasks and responsibilities are based on standard research guidelines, including standard operating procedures. Data sources are monitored and evaluated for case and control definition conformity, errors, and missing data at each sentinel site. Vaccination records, underlying diseases, medical history, radiological findings, and demographic characteristics are recorded prospectively for each patient on a case report form (CRF) (Table 3). Data quality reporting is redacted for each site to ensure the confidentiality and conformity of all study data variables. This process will be applied to data analysis of each enrolled case and control subject. Data accuracy will be assessed by comparing the recorded values with source documents. The principal investigator at each site is contacted for queries regarding this quality assessment and is involved in resolution.
Data analysis
An anonymous database will be built, and clinical data will be linked to laboratory data. Quantitative variables will be described and categorised according to their distribution in the study population. Descriptive analysis will address each covariate for the entire population and will be stratified by site. Patients’ characteristics and laboratory data for cases and controls will be compared. The associations between risk factors and carriage will also be examined by estimating the relative risk in the study population. Data analysis will be conducted using software such as R and SPSS. The absence/presence of SPN will be modelled using a mixed effects logistic regression model and random forest. The validity of the model will be tested using cross-validation. Sensitivity analysis will also be carried out to evaluate the impact of selected clinical and demographic parameters on the BinaxNOW test outcome.
Discussion
MY-Pneumo study collects data on potential risk factors that may influence trends in respiratory disease, as well as pneumococcal carriage among healthy controls. This study incorporates different study designs which will help us to interpret the changes over time in younger children with pneumonia following PCV10 introduction. The results obtained from this study will be reported in due course, with the hope that the information gained will contribute to a better understanding of pneumococcal disease in the Malaysian context. Regional site analysis, focusing on specific interests, will also be described and published at a later date. Study analysis will generally focus on the prevalence of pneumonia for the entire population and by the sentinel site. Insufficient data regarding pneumonia aetiology in developing countries is evident from the geographical distribution of study sites worldwide [13,14,15]. It has been suggested that further carriage and disease studies are required in middle-income countries, especially in Malaysia, to assess the effectiveness of pneumococcal vaccination to monitor serotype changes in the population [16,17,18]. The Pneumonia Etiology Research for Child Health (PERCH) study was the largest, most comprehensive pneumonia aetiology study conducted in seven countries in Africa and Asia: Gambia, Mali, Kenya, Zambia, South Africa, Bangladesh, and Thailand from 2011 to 2014 [19]. The study setting involved severe childhood pneumonia cases (4,232 children between 1 month and 5 years), and each country had different characteristics that may have influenced the causes of pneumonia. Yet, the research study was pivotal in advancing our understanding of the causes and contributors to childhood pneumonia in developing countries. By investigating a diverse range of variables and risk factors, the PERCH study contributed to driving transformative changes in child health outcomes, reducing the burden of pneumonia-related morbidity and mortality. A more comprehensive understanding of the pathogens responsible for childhood pneumonia holds the potential to significantly enhance both preventive measures, including the implementation of effective vaccine policies, and therapeutic interventions. This collective effort towards a better understanding of pneumonia causality has the power to drive improved management strategies, ultimately resulting in a remarkable reduction in the burden of morbidity and mortality associated with childhood pneumonia.
The present study’s main strength is the prospective multicentre case–control study design that will permit the description of paediatric pneumococcal pneumonia in study-related locations, especially in urban and rural areas. The sampling and laboratory methods used are consistent with other research studies that have described nasopharyngeal carriage in young children [19, 20]. Gold-standard molecular methods have been utilised to detect pneumococcus in the nasopharynx [21]. The use of the PUAT assay, which detects pneumococcal polysaccharides in the urine of young children, will enable rapid detection of pneumococcal antigens, allowing for timely intervention and reducing the risk of complications.
Whilst our study includes three states in both urban and rural community areas of Peninsular Malaysia, we did not include other states in East Malaysia. Therefore, our findings may not be applicable to represent the diversified population and demographics of Malaysia. The COVID-19 pandemic and co-infection status for pneumonia cases may impact study outcomes as we do not have administrative data available for both. However, we plan to incorporate this information whenever available into the descriptive interpretation of study results. Moreover, we do not have pneumococcal carriage data for the retrospective period and have therefore chosen clinical endpoints as our primary study objective.
This study will contribute to the incomplete evidence available on the burden of pneumococcal pneumonia in children below the age of 5 years in low-resourced countries, particularly in the Asia–Pacific region. Data on the burden of pneumococcal pneumonia and the impact of PCV can guide decisions related to vaccine prioritisation, resource allocation, and healthcare strategies. As PCV is being introduced in various low-resource settings to combat pneumococcal diseases, understanding its effectiveness and potential benefits is critical for public health strategies. The study is one of the few active population-based pneumonia surveillance programs evaluating the indirect impact of PCV in a resource-limited setting. With the increasing introduction of PCV in low-resourced settings, the methods, experiences, and lessons learned from our study may guide the development of such systems in other countries.
Availability of data and materials
Not applicable – manuscript does not contain any data.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- CBA:
-
Columbia agar with 5% sheep blood
- CDC:
-
Centers for Disease Control and Prevention
- CI:
-
Confidence interval
- COVID-19:
-
Coronavirus disease 2019
- cpsA:
-
The capsular polysaccharide biosynthesis gene A
- CRF:
-
Case report form
- CRP:
-
C-reactive protein
- CSF:
-
Cerebrospinal fluid
- CXR:
-
Chest radiograph
- DNA:
-
Deoxyribonucleic acid
- HUSM:
-
Hospital Universiti Sains Malaysia
- IMU-AMCRL:
-
International Medical University Advanced Microbiology Collaborative Research Laboratory
- IPD:
-
Invasive pneumococcal disease
- NIP:
-
National Immunisation Programme
- NPS:
-
Nasopharyngeal swab
- OR:
-
Odds ratio
- PCR:
-
Polymerase chain reaction
- PCV:
-
Pneumococcal conjugate vaccine
- PCV10:
-
10-Valent pneumococcal conjugate vaccine
- PERCH:
-
Pneumonia Etiology Research for Child Health
- PUAT:
-
Pneumococcal urine antigen test
- SASMEC IIUM:
-
Sultan Ahmad Shah Medical Centre International Islamic University Malaysia
- SPN:
-
Streptococcus pneumoniae
- STGG:
-
Skim milk, tryptone, glucose, and glycerol
- UMMC:
-
University Malaya Medical Centre
- WGS:
-
Whole-genome sequencing
- WHO:
-
World Health Organization
References
WHO. Pneumonia in children. 2022. Available from: https://www.who.int/en/news-room/fact-sheets/detail/pneumonia Cited 2023 Aug 17.
UNICEF DATA. neumonia in Children Statistics. 2022. Available from: https://data.unicef.org/topic/child-health/pneumonia/ Cited 2023 Aug 17.
Sutriana VN, Sitaresmi MN, Wahab A. Risk factors for childhood pneumonia: a case-control study in a high prevalence area in Indonesia. Clin Exp Pediatr. 2021;64(11):588–95.
Beletew B, Bimerew M, Mengesha A, Wudu M, Azmeraw M. Prevalence of pneumonia and its associated factors among under-five children in East Africa: A systematic review and meta-analysis. BMC Pediatr. 2020;20(1):254.
Bartlett JG, Dowell SF, Mandell LA, File TM, Musher DM, Fine MJ. Practice guidelines for the management of community-acquired pneumonia in adults. Clin Infect Dis. 2000;31(2):347–82.
Chee E, Huang K, Haggie S, Britton PN. Systematic review of clinical practice guidelines on the management of community acquired pneumonia in children. Paediatr Respir Rev. 2022;42:59–68.
Amin-Chowdhury Z, Aiano F, Mensah A, Sheppard CL, Litt D, Fry NK, et al. Impact of the Coronavirus Disease 2019 (COVID-19) Pandemic on Invasive Pneumococcal Disease and Risk of Pneumococcal Coinfection with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): Prospective National Cohort Study. England Clin Infect Dis. 2021;72(5):e65–75.
RIVM. The National Immunisation Programme in the Netherlands Surveillance and developments in 2019–2020. Netherlands; 2020.
Ng DCE, Tan KK, Ting GSS, Ling C, Fadzilah NFB, Tan SF, et al. Comparison of severe viral pneumonia caused by SARS-CoV-2 and other respiratory viruses among Malaysian children during the COVID-19 pandemic. Front Pediatr. 2022;10:865099.
Cherian T, Mulholland EK, Carlin JB, Ostensen H, Amin R, De Campo M, et al. Standardized interpretation of paediatric chest radiographs for the diagnosis of pneumonia in epidemiological studies. Bull World Health Organ. 2005;83(5):353–9.
CDC Streptococcus Laboratory. NCIRD/DBD/RDB-Centers for Disease Control and Prevention. 2010. Streptococcus pneumoniae carriage study protocol ‐ nasopharyngeal (NP) swab processing. Available from: https://www.cdc.gov/streplab/pneumococcus/resources.html#carriage-protocols Cited 2023 Aug 17.
Bankevich A, Nurk S, Antipov D, Gurevich AA, Dvorkin M, Kulikov AS, et al. SPAdes: A new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol. 2012;19(5):455–77.
Ali H, Aziz S. Rising Pediatric Morbidity and Mortality in the Developing World. Cureus; 2021.
Nathan AM, Teh CSJ, Jabar KA, Teoh BT, Tangaperumal A, Westerhout C, et al. Bacterial pneumonia and its associated factors in children from a developing country: A prospective cohort study. PLoS ONE. 2020;15(2):e0228056.
Rudan I, Boschi-Pinto C, Biloglav Z, Mulholland K, Campbell H. Epidemiology and etiology of childhood pneumonia. Bull World Health Organ. 2008;86(5):408–16.
Tricarico S, McNeil HC, Head MG, Cleary DW, Clarke SC. Informing pneumococcal conjugate vaccine policy in middle-income countries: The case of Malaysia. Vaccine. 2017;35(18):2288–90.
Tricarico S, McNeil HC, Cleary DW, Head MG, Lim V, Yap IKS, et al. Pneumococcal conjugate vaccine implementation in middle-income countries. Pneumonia. 2017;9(1):6.
Lister AJJ, Dombay E, Cleary DW, Sulaiman LH, Clarke SC. A brief history of and future prospects for pneumococcal vaccination in Malaysia. Pneumonia. 2023;15(1):12.
O’Brien KL, Baggett HC, Brooks WA, Feikin DR, Hammitt LL, Higdon MM, et al. Causes of severe pneumonia requiring hospital admission in children without HIV infection from Africa and Asia: the PERCH multi-country case-control study. Lancet. 2019;394(10200):757–79.
Picot VS, Bénet T, Messaoudi M, Telles JN, Chou M, Eap T, et al. Multicenter case-control study protocol of pneumonia etiology in children: Global Approach to Biological Research, Infectious diseases and Epidemics in Low-income countries (GABRIEL network). BMC Infect Dis. 2014;14(1):635.
Satzke C, Dunne EM, Porter BD, Klugman KP, Mulholland EK, Vidal JE, et al. The PneuCarriage Project: A Multi-Centre Comparative Study to Identify the Best Serotyping Methods for Examining Pneumococcal Carriage in Vaccine Evaluation Studies. PLoS Med. 2015;12(11):e1001903.
Acknowledgements
The authors thank all staff nurses and medical officers from the sentinel sites for their valuable contributions to this study. The authors also would like to thank all the parents/legal guardians and children who participated in the study.
Funding
This work is funded in part by a research grant from the Investigator Initiated Studies Program of Merck Sharp & Dohme Corp (MSIP #60200). The funding body did not play any role in data collection, decision to publish, or drafting of the manuscript. The opinions expressed in this paper are those of the authors and do not necessarily represent those of Merck Sharp & Dohme Corp.
Author information
Authors and Affiliations
Contributions
All authors designed and co-authored the protocol. NHR and ATCH were responsible for preparing the manuscript. LHS and SCC conceived the idea. LHS, SCC, CCW, NHR, and NAJ drafted the original proposal. CSJT, SNHH, ZZD, and NK supported microbiological aspects-based protocols. AMN, NAS, MII, ZZD, NSMN, AAB, MAMH, and WKWJ coordinated study implementation at sentinel sites. DWC supported the WGS analysis. All authors read, commented on, and approved the final manuscript version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol, informed consent statement, case report form, any amendments and all other study documents have been submitted to and approved by the institutional ethics committee of each site:
-
1.
The International Medical University Joint-Committee on Research & Ethics (4.15/JCM-216/2021),
-
2.
The Human Research Ethics Committee, Universiti Sains Malaysia (USM/JEPeM/21020190),
-
3.
The International Islamic University Malaysia Research Ethics Committee (IREC 2021–114), and
-
4.
The Medical Research Ethics Committee, University Malaya Medical Centre (MREC ID No: 2021128–9769)
-
5.
University of Southampton's Ethics and Research Governance (ERGo II 64844)
Consent for publication
Not required because no individual identifiers have been included in the manuscript.
Competing interests
DWC was a post-doctoral researcher on GSK funded projects in 2014/15 and has received grant support from Pfizer and the National Institute for Health via the NIHR Southampton Biomedical Research Centre. LHS and SCC act as principal investigators for clinical trials and other studies conducted on behalf of IMU University, and University Hospital Southampton NHS Foundation Trust/University of Southampton, respectively, that are sponsored by vaccine manufacturers. No personal payments are received from them. SCC has participated in advisory boards for vaccine manufacturers but receives no personal payments for this work. NHR and SCC have received financial assistance from vaccine manufacturers to attend conferences. All grants and honoraria are paid into accounts within the respective IMU University and NHS Trusts or Universities, or to independent charities. All other authors have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ramzi, N.H., Hoong, A.T.C., Johari, N.A. et al. Multicentre case–control study of pneumococcal infections among children with pneumonia in Peninsular Malaysia (MY-Pneumo): a study protocol. BMC Public Health 24, 2255 (2024). https://doi.org/10.1186/s12889-024-19789-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19789-9