- Research
- Open access
- Published:
Posttraumatic growth of medical staff during COVID-19 pandemic: A scoping review
BMC Public Health volume 24, Article number: 460 (2024)
Abstract
Background
The COVID-19 pandemic has imposed unprecedented stress and challenges upon medical staff, potentially resulting in posttraumatic growth (PTG). This scoping review aims to synthesize the existing knowledge on PTG among medical staff during the pandemic by identifying its current status and potential influencing factors. The findings may provide a foundation for future research and interventions to enhance the medical staff’s psychological resilience and well-being.
Methods
Literature was systematically searched on PTG among medical staff during the COVID-19 pandemic from 01 January 2020 to 31 December 2022. The following databases were searched: PubMed, Web of Science, Embase, CINAHL, PsycINFO, Cochrane Library, China National Knowledge Infrastructure (CNKI), Chinese Biomedical Literature Service System (SinoMed), and Wanfang Data. Eligibility criteria included: (1) medical staff as research subjects; (2) a focus on “posttraumatic growth” or “alternative posttraumatic growth” related to the COVID-19 outbreak and pandemic; (3) discussion of the situation and influencing factors of PTG; and (4) study types, such as qualitative, quantitative, and mixed methods. Two researchers independently selected and extracted study characteristics (study design, study population, region, measurement instruments, and primary outcomes) from the included literature. The data were synthesized qualitatively and descriptively.
Results
Thirty-six papers from 12 countries met the inclusion criteria. Moderate PTG levels were observed among healthcare workers during the COVID-19 pandemic, with emphasis on “interpersonal relationships,” “changes in life philosophy,” and “growth in personal competence.” Influencing factors included trauma exposure, sociodemographics, psychological characteristics (resilience and positive qualities), coping, and social support.
Conclusions
This review discovered moderate PTG levels among medical staff during the COVID-19 pandemic, with critical areas in interpersonal relationships, life philosophy, and personal competence. The identified influencing factors can inform future research and interventions to enhance healthcare workers’ psychological resilience and well-being.
Introduction
Posttraumatic growth (PTG) has been defined as “positive psychological change that occurs following a struggle with highly challenging life circumstances” and through establishing perspectives for a “new normal” when the old normal is no longer an option [1]. The positive transformation developed five domains: development of deeper relationships, openness to new possibilities, a greater sense of personal strength, a stronger sense of spirituality, and a greater appreciation of life; followed by the development of the Posttraumatic Growth Inventory (PTGI), which has been translated into more than 20 languages and extensively validated worldwide [1, 2]. PTG is associated with PTGI across numerous cultures and many different traumatized populations, including those who have survived natural disasters [3], bereavement [4], cancer [5], human immunodeficiency virus (HIV) [6], suicide [7], assault [8], refugee [9], and combat veterans [10], and so on.
Furthermore, people with a strong connection to trauma victims, such as health personnel, family members, caregivers, social workers, and psychotherapists, have also demonstrated vicarious posttraumatic growth (VPTG) in the context of secondary trauma or alternative trauma [11]. It is particularly prevalent among professionals working with trauma survivors. They may experience personal and professional growth due to witnessing their clients’ resilience and ability to overcome adversity. These experiences include positive changes in self-cognition, interpersonal relationships, life values, increased compassion, sensitivity, and insight [12], and extraordinary growth in the context of one’s professional identity, which is professional’s job satisfaction and self-competence by witnessing the growth of their clients [13, 14].
The novel coronavirus (COVID-19) pandemic has had a profound global impact since its discovery in December 2019. As of March 11, 2023, the World Health Organization (WHO) has reported that the cumulative global cases of COVID-19 have surpassed 759 million, with nearly 6.9 million deaths [15]. Despite the WHO’s announcement on May 5, 2023, that the COVID-19 pandemic will no longer be classified as a global public health emergency, it is important to note that the threat to global health has not been eradicated. With the lifting of the state of emergency, it is imperative to address the psychological ramifications stemming from the pandemic [16]. The global healthcare system has been strained by the pandemic, placing a significant burden on healthcare workers (HCWs), particularly those in direct contact with COVID-19-diagnosed patients. This has resulted in a range of mental health issues, including pain, anxiety, burnout, depression, insomnia, posttraumatic stress disorder (PTSD), denial, and fear, which have adversely affected medical personnel, regardless of their direct or indirect exposure to trauma [17]. Despite the difficulties encountered, healthcare professionals can endeavor to adapt to demanding circumstances and rebound from traumatic experiences, which may result in favorable outcomes such as posttraumatic growth (PTG) or vicarious posttraumatic growth (VPTG). This inherent resilience among medical personnel is underpinned by their specialized training and extensive experience in crisis management, enabling them to navigate the uncertainties and pressures associated with the COVID-19 pandemic [18]. Furthermore, the daily exposure to life-and-death situations, coupled with a strong sense of professional duty, equips healthcare workers with the capacity to maintain composure and professionalism even in the face of overwhelming challenges [19]. These qualities not only facilitate their ability to cope but also lay the foundation for potential positive psychological outcomes such as PTG. Therefore, the exploration of PTG becomes integral in understanding how healthcare professionals not only withstand the adversities brought about by the pandemic but also use these experiences as catalysts for personal and professional development. The study of PTG is crucial not just for mitigating the negative psychological consequences of trauma but for promoting a resilient healthcare workforce, capable of not only enduring but thriving in the aftermath of significant challenges.
To the best of our knowledge, existing research on the level of PTG and its influencing factors among medical staff has presented some variability across different regions during the COVID-19 pandemic. A preliminary search for existing scoping reviews in systematic review databases, such as JBI, Cochrane, TRIP database, and PROSPERO, on 01 October 2022, revealed no systematic reviews or scoping reviews on this topic or any currently in progress. Consequently, this study, grounded in the scoping review methodology of Arksey and O’Malley [20], aims to (a) map the prevalence and characteristics of PTG in healthcare settings during the COVID-19 pandemic (b) identify key factors that may influence its development and (c) highlight the knowledge gaps for future research and interventions aimed at enhancing the psychological resilience and well-being of healthcare workers in the face of public health crises.
Methods
This scoping review followed the scoping review framework developed by Arksey and O’Malley [20], including five stages: (1) identifying the research questions; (2) identifying relevant studies; (3) study selection; (4) charting the data; and (5) collating, summarizing and reporting the results. The results were based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Extension for Scoping Reviews (PRISMA-ScR) checklist [21]. The PRISMA-ScR was intended to guide the reporting of this scoping review based on the relevance, credibility, and contribution of evidence. The completed PRISMA-ScR checklist can be found in Additional file 1.
Search strategy
The literature was systematically reviewed between 01 January 2020 and 31 December 2022 using the following databases: PubMed, Web of Science, Embase, CINAHL, PsycINFO, China National Knowledge Infrastructure (CNKI), Chinese Biomedical Literature Service System (SinoMed), and Wanfang Data. A search strategy was developed by combining key and MESH terms by two research team members. The third member approved it of the research team and finally confirmed it by consulting the medical librarian. Here are the specific details: “COVID-19“[Mesh], “SARS-CoV-2“[Mesh], “COVID-19”, “SARS-CoV-2”, “coronavirus disease 2019”, “2019n-cov”; “Posttraumatic Growth, Psychological“[Mesh], “posttraumatic growth”, “post-traumatic growth”, “vicarious posttraumatic growth”, “secondary posttraumatic growth”, “alternative posttraumatic growth”; “Medical Staff“[Mesh], “Health Personnel“[Mesh], “Healthcare workers”, “health care provider”, “front line workers”, “medical workers”, “medical staff”, “healthcare professionals”, “nurse*”, “doctor*”, “physician”, “paramedic”, and adjusted in each database. The medrxiv.org and the references cited by the retrieved articles were also searched for additional references. The search strategies are detailed in Additional file 2.
Study selection and eligibility criteria
Inclusion criteria were as follows: (1) the population described in the literature consisted of HCWs, including doctors, nurses, and other medical personnel who were directly or indirectly involved in the diagnosis, treatment, or care of patients with confirmed or suspected cases of COVID-19; (2) the research topic was “posttraumatic growth” or “alternative posttraumatic growth” associated with the COVID-19 outbreak and pandemic; (3) the situation and influencing factors of PTG were discussed in the literature; and (4) the study types included qualitative, quantitative, and mixed methods studies.
Exclusion criteria were as follows: (1) participants were medical students in clinical placement; (2) the study type was an intervention study; (3) the literature types were research protocol, conference literature, case reports, reviews, official reports, book reviews, letters to the editor, editorials, and studies published in preprint servers but not in peer-reviewed journals; and (4) duplicate and unavailable full-text, non-Chinese and non-English literature.
Data extraction
The retrieved literature was imported into the NoteExpress software, and duplicates were checked. The title and abstract of citations were independently reviewed by two reviewers for the first screening level to identify articles that met the minimum inclusion criteria. A subsequent review of the full-text articles was conducted by two reviewers for the second screening level. Studies were excluded if they did not meet the eligibility criteria or were unrelated to the research question and purpose. Disagreements were discussed with a third researcher and resolved by consensus if there were any disagreements and uncertainties relating to study selection.
A form was developed to confirm the relevance and extract study characteristics from the included sources of evidence. Then, two reviewers independently charted the extracted data from each eligible article, and disagreements among reviewers were discussed. This process aimed to create a descriptive summary of the results, including aims, study design, nation, participants, tools/method, and main findings.
Evidence was combined qualitatively and descriptively after collecting the relevant data. The similarities and differences between the included studies, their relationship, situation, and risk factors of PTG were reported.
Data integration methodology
This study employed a rigorous data integration approach to systematically synthesize and compare the results obtained from quantitative and qualitative research. This integration process aimed to gain a comprehensive understanding of PTG among medical staff during the COVID-19 pandemic. The following steps were adopted: (1) Identification of Common Themes: A detailed analysis of quantitative studies was conducted to identify key themes and patterns related to the characteristics and influencing factors of PTG. Concurrently, qualitative studies were thoroughly reviewed, employing content analysis to extract detailed individual experiences and nuanced insights on PTG. (2) Comprehensive Comparison: A comprehensive comparison table was established, encompassing the key statistical outcomes from quantitative research and the main themes from qualitative research. This table visually highlighted the consistencies and differences between the quantitative and qualitative research in terms of PTG characteristics and influencing factors. (3) Synthesis of Research Findings: The common themes from both research methodologies were synthesized. This included combining trends from quantitative data with profound insights from qualitative data to reveal a more comprehensive picture of PTG. Additionally, a detailed comparison and discussion were conducted to understand the perspectives and experiences captured by each research method in terms of PTG features and influencing factors. (4) Verification of Integrated Results: To ensure the accuracy and reliability of the integration process, the synthesized results were subjected to rigorous review by multiple researchers.
Results
Search results
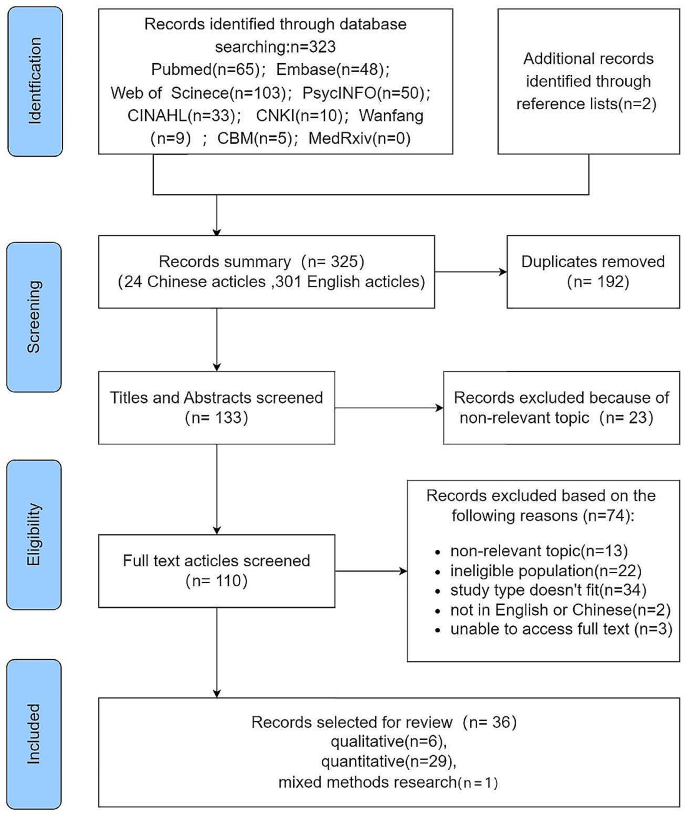
The primary search discovered 325 papers, including 24 Chinese and 301 English articles. After removing duplicates, 133 papers were left. We selected 110 articles for full-text reading based on screening titles and abstracts. We excluded 74 articles due to unrelated topics (n = 13), ineligible study populations (n = 22), noncompliant study designs (n = 34), not in English or Chinese (n = 2), and unobtainable full texts (n = 3). Finally, our analysis included 36 studies. Figure 1 presents a flowchart of the search strategy and the selection process based on identified criteria.
Characteristics of sources of evidence
Five of the 36 articles were in Chinese, with the remaining 31 in English. Three were published in 2020, 15 in 2021, and 18 in 2022 (one of the studies was online in 2022 and published in 2023). The study included18 articles from China, four from Turkey, three from the United States, three from Korea, one from other countries, such as Greece, Italy, Canada, Spain, Israel, Serbia, and Palestine, and one from a global study covering three countries (Israel, Canada, and France).
The study population included 17 papers on frontline medical staff (care for COVID-19-diagnosed patients), four papers on nurses diagnosed with COVID-19 infection, and 15 on medical workers. It involves the emergency department, intensive care unit, dentistry, psychiatric department, and outpatient department. The medical institutions involved hospitals designated to treat patients diagnosed with COVID-19, general hospitals, communities, clinics, and other hospitals. The PTG level was measured at one to three-time points in 23 cross-sectional and six longitudinal studies, primarily using online questionnaires. Six qualitative articles utilized semi-structured interviews and questionnaires via telephone, video, or face-to-face interviews. Scale and open-question surveys were used in one mixed mothed record. Table 1 represents the general characteristics of the included literature.
Synthesis of results
Quantitative results
The level of posttraumatic growth
The Posttraumatic Growth Inventory (PTGI), a 21-item scale developed by Tedeschi and Calhoun [2] in 1996, measures PTG, including five dimensions: relationship with others, new possibilities, personal strength, spiritual change, and appreciation of life. It is scored on a 6-point Likert scale from 0 to 5, ranging from “not at all” to “very much.” Researchers in various regions have modified this scale based on cultural adaptation. Most Chinese studies used the revised version of the 20-item PTGI by Wang Ji [58], deleting item 18, “My religious beliefs are stronger,” due to its low correlation with the total score and local culture in China. It adopted the Likert 6-point scale with a score of 0–100. Six studies [28, 32, 36, 37, 43, 44] used a 10-entry short version of the PTGI scale (PTGI-SF), adopting a Likert 6-point scale with a total score of 0 to 50 [59]. Tedeschi et al. [60] updated the list with four new items in the spiritual and existential change subscale to better capture spiritual and existential change in non-religious cultures, comprising PTGI-X with 25 items scored from 0 to 125 with a 6-point Likert scale. Two studies included in this review used it as a measurement [25, 55]. PTG levels reached moderate and above with mean item scores of PTGI > 3 or total scores > 60 in two studies [24, 38]. However, another study indicates that people who scored higher than the 60th percentile might have grown [37].
HCWs experienced varying PTG levels following direct or indirect trauma during the COVID-19 epidemic. A total of 28 studies in the included literature reported specific PTGI scores, with moderate PTG levels in general and high scores on the dimension of “relating to others”, “appreciation of life”, and “personal strength” more frequently mentioned. Table 2 presents the details.
The influencing factors of posttraumatic growth
Trauma
COVID-19 could be categorized as a new type of mass trauma. Different types of trauma-related scenarios or characteristics may influence PTG levels. COVID-19-exposed HCWs, such as those working in intensive care units (ICUs) or frontline or sentinel hospitals where confirmed cases are treated, had higher PTG levels [23, 29, 37, 45, 51]. HCWs diagnosed with COVID-19 or have a family member, friend, or colleague who has been diagnosed had higher PTG levels [51, 56].
The PTG levels of HCWs differed at different stages of the COVID-19 pandemic. A longitudinal study of frontline HCWs (n = 134) in China showed that Time 1 (Feb 2020) to Time 2 (Mar 2020) participants revealed an increase in PTG, while Time 3 (May 2020) participants indicated a decrease in PTG [42]. Another three-wave longitudinal study (n = 565) from China discovered that PTG gradually increased over two years of follow-up among HCWs, and four types of PTG trajectory were identified: persistent, steady increase, high with a drop, and fluid trajectory [22]. However, one study (two-point survey) from Turkey indicated that PTGI scores decreased significantly over time among 66 HCWs participated in the study [24]. Another two-wave survey from the U.S. radiology staff revealed a consistent trend toward lower PTGI [23].
The severity of the traumatic event and PTG in HCWs may have a positive or negative correlation. Researchers have also discovered that PTG was negatively correlated with trauma [28] and PTSD symptoms [47]. Another study indicated that PTG was positively correlated with PTSD [36].
Demographic characteristics
Gender, age, work years, job title, education level, marital status, child status, religion, and race may be associated with PTG. Most studies discovered higher PTG levels among HCWs with older age [22, 23], longer working years [33, 38], higher job titles [51], and higher education levels [22, 51]. However, some studies revealed that PTG was negatively correlated with age [25, 34] and professional title [47]. Not coincidentally, gender differences were also observed across studies. A survey of 455 nurses from China indicated that women had lower PTGI scores than men [29]. A survey of 673 HCWs from Greece showed that women scored higher on all VPTG subscales [34]. However, another large (n = 12,596) study from China demonstrated a greater trauma response in women than in men but no difference in PTG [37]. Similarly, a study from Serbia produced consistent results [56].
Additionally, HCWs with religious beliefs [32, 33], married [29], with children [39], and working part-time [32] had higher PTG levels. PTG levels differed between physicians and nurse assistants [43], and whether they were white [36] or born locally also differed from PTG levels [33]. Disaster training, rescue, critical patient resuscitation, and infectious disease treatment experience contribute to a higher PTG level [51].
Psychological factors or personal traits
Positive emotions or psychology or personal traits can promote PTG, such as resilience [22, 26, 33, 42], occupational resilience [50], occupational identity [45], self-efficacy [47], deliberate rumination [30, 38, 55], subjective well-being [28], coherence [28], harmonious passion [43], frontline job confidence [38], risk awareness [38], transformative power of pain [31], trust, reciprocity, and identification [41], being psychological comfort [39], and positive emotions and dispositional gratitude [36], as mentioned in most studies.
Negative emotions or psychological or personal traits can inhibit the PTG onset; examples include COVID-19-related stress/anxiety/concern [28] and job burnout [28, 42]. However, similar to trauma, the stress/anxiety/concern associated with COVID-19 has also revealed a double-edged sword effect on PTG. For instance, research from China exhibited that higher COVID-19-related worries and psychological distress meant a higher PTG level [32]. Studies from other regions have demonstrated the same effect [43, 44]. An increased stress mindset, determining the stress response, is associated with higher PTG levels [25].
Coping and social support
A positive coping style can contribute to PTG, including conducting psychological interventions/training, engaging in online counseling, and phone app of application self-relaxation [25, 29, 38, 47, 56].
A positive association has been demonstrated between PTG and social support, including support from organizations [26, 50], societies [30, 45, 47, 53], families [39, 52], and friends [39]. Additionally, good working relationships, such as nurse-patient satisfaction [51] and job satisfaction [32], can promote PTG in HCWs.
Seven studies explored the path analysis of the PTG influencing factors and discovered the mediating and moderating factors under their respective theoretical models, such as organizational support [50], social support [30, 57], coping strategies [25, 34], resilience [53], psychological security [41], expressive suppression [53], deliberate rumination [30], emotional exhaustion [42], self-disclosure [30], and positive psychological capital [57].
Qualitative results
Six qualitative studies [27, 35, 40, 46, 48, 54] described the specific experiences of HCWs when confronted with or diagnosed with COVID-19 through three periods of stress/negativity, adjustment to adaptation, and growth, presenting PTG occurrence. The qualitative part of another mixed study [49] identified three themes: quality of workplace relationships, sense of emotional-relational competence, and clinical-technical competence. Each theme has two broad macro categories: growth and block.
Change in relationships with others
Six of the Seven studies contributed to this theme. Improved interpersonal relationships include with family, friends, colleagues, and patients. Family, friends, and colleagues’ warm love and support bring their relationship closer and more intimate. A nurse diagnosed with COVID-19 remarked, “My boyfriend cared for me, encouraged me, and gave me strength after I got sick; I will cherish the relationship between us” [54]. “When I saw my son at the gate of the community after I came back from isolation, I burst into tears and held him tightly in my arms” [27]. As healthcare worker spends more time with a patient, their empathy and compassion for the patient gradually intensifies. Like comrades who fought back the “enemy” (COVID-19), both sides cheered and encouraged each other to overcome difficulties and diseases, improving the relationship between doctors and patients. One nurse said, “When the test result returned negative for the first time after being admitted, I was so happy and cried together with the patients” [48]. Additionally, the experience of being a patient after a COVID-19 diagnosis also influences how HCWs treat patients, and role reversal and empathy improve the relationship with patients to some extent [27, 54]. During this particular time, colleagues’ help, care, and encouragement in caring for infected patients promote teamwork and interpersonal relationships [27, 35, 48, 49, 54].
Increase in individual strength
This resulted in a shift in participants’ mental and professional perceptions of themselves. At a psychological level, HCWs reported that the experience had made them more courageous, strong, and optimistic. “I think I am a little more brave and strong than I thought I would be” [54]. In the face of difficulties or trauma, resilience allows individuals to make positive choices and respond rationally to stress. This facilitates guiding individuals to reconstruct non-adaptive states and activate their potential to resist crises to resolve difficulties. Most HCWs described their experiences exploring and reconfiguring their strengths [27].
At the professional level, HCWs had a positive attitude toward gaining work experience related to a new infectious disease [48, 49]. They viewed their current experience as a valuable opportunity to learn new skills and enhance their work, gradually moving from unfamiliarity at the beginning to completing the work previously given to the nurse aides and being able to quickly shift and focus on enhancing the quality of care and improving patient well-being. This adds significance to their experience [48].
Changes in the philosophy of life and priorities
Four of the seven studies contributed to this theme. Interviewees mentioned a new appreciation of life and the future after experiencing trauma. They will re-examine life’s meaning and re-plan their future priorities, such as“I felt the need to live more meaningfully as the disease gave me another chance to live. I became more attached to life and realized how valuable it is …” [40].
Most life priorities change are reflected in the increased priority given to physical health. “Nothing is better than a healthy life, and nothing is as important as health” [27]. “… I realized that health is more important than anything else. Thus, I decided to stop worrying about some things, stop overthinking, and stop to give importance. I realized that health is the most important thing” [40]. Moreover, it is reflected in other meaningful and fun things, such as “I will get better for myself and my family. I will spend more time with them, cherish every day, and enjoy the fun of life. I still have many important tasks to complete” [27].
Self-identification of profession
Participants in four studies described greater vocational identity. Most participants expressed satisfaction and pride that they were making a concrete contribution to the fight against the global pandemic. Their pride was further enhanced with increased social recognition of HCWs caring for COVID-19 patients. All of these enhanced their professional identity. “The work that I am doing is truly helping others. I am contributing during this national disaster situation. I am here at this historical moment…” [48], “I am proud to be a nurse and to have assisted on the front lines” [35], and “I think every HCW is a hero” [54]. As child and adolescent psychiatrists, they have experienced a successful transition from “who we are” and “what we can do now” to “who we will become” during the pandemic and then engendered a reevaluation of and a recommitment to psychiatry [46].
Spiritual change
One research reported a change in spirituality [40]. After being diagnosed with COVID-19, the nurses questioned their spiritual lives and changed. “Inevitably, death anxiety enters your mind, and you question yourself. I realized how spiritually weak I was and made a promise to myself. I would pay more attention to my prayers after the treatment … I was angry with myself as I was living in this way….” “Thus, I realized that everything was in vain; the only real thing is after death. … I started to question my mistakes and sins and plan to get rid of them … I turned to God more.” Many of them rely on religious beliefs to manage stress.
Integration of quantitative and qualitative research
To provide a clearer understanding of the consistency and divergence between quantitative and qualitative studies in the PTG of HCWs, we have established Table 3 to compare the associations of these two research methods regarding PTG characteristics and influencing factors.
Through the comparison presented in the table, we observe a notable coherence and complementarity in understanding the characteristics and influencing factors of PTG among HCWs during the COVID-19 pandemic. In terms of PTG characteristics, the themes distilled from qualitative studies correspond closely with the five dimensions measured in quantitative PTG scales. This alignment elucidates the specific contexts and manifestations of these dimensions, providing a clearer and more comprehensive understanding of what PTG looks like for HCWs in the context of the pandemic. Regarding influencing factors, there is a synergistic relationship between the themes identified in qualitative research and the factors statistically derived from quantitative studies. For instance, qualitative themes such as “Work-related stressors” and “Psychological stress and emotional reactions” offer a vivid explanation of HCWs’ early responses to the “Trauma” of the COVID-19 pandemic. Additionally, qualitative findings explicate how internal and external factors foster PTG, detailing the process of its formation. This consistency and complementarity between qualitative and quantitative approaches highlight the importance and value of employing a combined methodological perspective for a holistic understanding of PTG.
Discussion
This literature review aimed to provide insight into the existing evidence base of what PTG looks like in HCWs and internal and external factors that may contribute to and hinder this phenomenon.
Summary of findings
Thirty-six papers from 12 countries met the inclusion criteria. In the context of the COVID-19 pandemic, HCWs faced tremendous stress and strain, generating associated mental health problems. They were also stimulated to adapt and adjust, generating PTG; the most notable included “interpersonal relationships,” “changes in life philosophy,” and “growth in personal power”. The factors influencing PTG were the level of trauma exposure, sociodemographics, and the psychological traits of the traumatized individual, such as psychological resilience, positive psychological qualities, and coping and social support.
Integrated discussion
Our study reveals the alignment and complementarity between qualitative and quantitative research. The integration of these methodologies not only enriches our understanding of PTG’s features but also enhances our grasp of its complexity. The themes identified in qualitative research correspond to the dimensions of the PTGI used in quantitative studies, elucidating the specific contexts and manifestations of these dimensions within the healthcare environment. For example, the growth in the personal strength dimension of PTGI, when reflected in the workplace, manifests as enhanced skills, increased confidence, professional identity, and a sense of accomplishment [46, 48, 54]. Moreover, the detailed backgrounds and descriptions provided by qualitative research help explain how factors identified in quantitative studies facilitate PTG. For instance, quantitative data may show a correlation between social support and increased PTG, but qualitative insights explain the mechanisms and reasons behind these relationships [27, 48, 54].
Qualitative research, with its intricate depiction of the phenomenon, addresses the limitations of quantitative research, enriching our understanding across various dimensions. This profound understanding aids in a more nuanced grasp of the essence and complexity of posttraumatic growth. Ultimately, this integrative approach not only broadens our comprehension of PTG but also underscores the value of combining qualitative and quantitative methods in mental health research. It provides a blueprint for future studies, demonstrating the importance of methodological diversity for a comprehensive understanding of complex psychological phenomena.
What does posttraumatic growth look like?
The variation in cultural backgrounds, measurement instruments, dimensions, and the reliability and validity of PTG assessments made it difficult to compare specific values across studies. Discrepancies in PTG levels might also be attributed to differences in survey time frames, health service contexts, pandemic control measures, and individuals’ subjective appraisals of COVID-19-related stressors. The criteria for classifying different PTG levels varied across studies. Several studies [24, 37, 38] used total scores > 60, single entry scores > 3, or ≥ 60% of the total scores as an intermediate or higher level of PTG, while others did not report delineation criteria. Overall, a medium level of PTG was observed. The COVID-19 pandemic has imposed enormous stress on HCWs, leading to mental health problems. Nevertheless, they adapt and adjust, ultimately yielding positive behaviors and experiences. The pandemic prompted the most profound changes in “human relationships,” “philosophy of life,” and “personal strength,” consistent with the qualitative studies review.
After experiencing an initial period of negative emotions in response to acute stress, individuals mobilize internal and external resources to manage the effects of trauma. Internal resources, such as mental toughness, intentional reflection, and resilience, with external resources like organizational, familial, and societal support, contribute to the positive outcome known as growth [61]. During this process, support from others facilitates adaptation and adjustment while manifesting in growth expressions, enhancing relationships, and creating reciprocal influence. After the trauma, individuals develop a positive and transcendent view of themselves and a new philosophy of life, appreciating various aspects, including health, existence, subtle experiences, and relationships.
What affects posttraumatic growth?
Trauma
The COVID-19 pandemic, as a traumatic event, has disrupted the assumptive world of HCWs, leading to their dysregulated cognitions and emotions. However, according to the model of “Posttraumatic Growth at Work” [52], they may achieve PTG via a recursive cycle of emotion regulation and sensemaking.
First, individuals with high trauma levels of exposure may exhibit severe PTSD symptoms, but higher trauma levels of exposure do not necessarily imply higher growth levels. There is no PTG without trauma for individuals. However, mild trauma may be insufficient to stimulate growth, and severe trauma may be more detrimental than beneficial to growth [62]. Thus, only moderate trauma exposure may trigger individual PTG and provide room for growth, demonstrating a positive correlation. For instance, a study discovered a linear and curvilinear relationship between trauma and posttraumatic development, and moderate indirect trauma was associated with the highest PTG levels [63]. A network analysis of war-related PTG revealed a U-shaped relationship between posttraumatic stress symptoms (PTSS) and PTG levels [9]. Additional studies supported these findings. The work experience of inpatient psychiatric nurses was associated with higher PTSD levels and secondary trauma. However, their growth was significantly slower compared to community nurses, which were thought to be associated with higher and continuous exposure to trauma and fewer opportunities to take breaks to reflect on it [64].
Second, although traumatic events are transient, their effects are continuous and dynamic, and post-traumatic stress and growth levels can change over time. For instance, a longitudinal study of tsunami survivors discovered that PTG could moderate the relationship between posttraumatic stress, depression, and quality of life after natural disasters [65]. Another tracking survey of earthquake survivors revealed that growth could reduce long-term PTSS [66]. Survivors may undergo self-adjustment and receive external support or intervention during the post-trauma period, which can accumulate over time and lead to different levels of trauma and growth. Their relationship remains uncertain due to the complex symbiotic relationship between trauma and growth and the many factors involved [67, 68].
Demographic characteristics
Although there are differences in the relationship between age, years of work, job title, education level, marital status, parental status, whether they were born in the local area, and PTG, they all share common factors that influence their growth. HCWs with more internal and external coping resources and a greater ability to cope with trauma exhibit higher PTG levels. Higher age, higher job title, higher years of work experience, and higher education level mean more internal resources, such as work experience and life experience, allowing them to use their clinical skills, integrate external resources through reflection, and then adopt a positive coping approach when faced with an unexpected pandemic. However, some studies also proved a negative correlation between age and growth [25, 34]. It might result from young people’s greater willingness to change their cognitive patterns and derive positive meaning from trauma, consistent with previous research on age differences in PTG [69]. Being married and having children may provide more emotional and material support resources from the family system, leading to higher PTG levels. According to other studies, the relationship between gender and PTG differs between studies [29, 34, 37], possibly due to the influence of other factors, such as the gender interaction with pandemic duration and individual quarantine [70].
HCWs who have received disaster training, rescue experience, critical patient resuscitation experience, and infectious disease treatment experience exhibit greater composure when faced with COVID-19. They can utilize their professional skills effectively to provide better care for critically ill patients and even lead other HCWs to do the same. This strengthens their sense of professional identity and honor and is associated with higher PTG levels [51].
Additionally, religiously engaged healthcare professionals have been shown to effectively use their faith and spirituality to cope with adversity during disasters. Religious beliefs can provide a framework to positively view threatening situations, facilitating a sense of challenge and growth through suffering [71]. Previous research has also highlighted the social support function of religious involvement [72]. Part-time nurses have higher PTG levels than full-time nurses [32]. This could be due to the extra time part-time employees must devote to their nursing duties and stressful experiences, potentially contributing to PTG.
Demographic characteristics may be associated with an individual’s emotional regulation and psychological resources in response to traumatic events. When designing interventions, the influence of these sociodemographic characteristics on PTG should be considered. Understanding these features carries significant practical implications for promoting PTG.
Psychological factors or personal traits
Regarding the temporal course of post-traumatic experiences, it has been suggested that intrusive rumination in the early stages of trauma can exacerbate psychological distress, elicit negative emotions and outcomes, and hinder PTG. However, as time progresses, an individual’s positive psychological resources, such as positive worldviews (hope, tolerance, psychological resilience, optimism, self-esteem, wisdom, and spirituality), positive emotions (happiness, gratitude, and satisfaction), and positive attitudes towards society (social cohesion, altruistic behavior, social responsibility, and benevolence), can aid in overcoming negative emotions and enhancing coping abilities [73]. Intrusive rumination may give way to active reprocessing and constructive thinking about the traumatic event under the influence of positive self-adjustment and social support. Moreover, negative reviews in the early stages of trauma can provide material for subsequent positive processing, enabling individuals to discover the positive meaning of the traumatic experience, ultimately promoting growth.
Psychological resilience, also known as resilience, refers to the ability to adapt or recover from highly adverse circumstances. It is a source of strength that enables individuals to remain well-adjusted, develop, and grow, and a key factor influencing whether they can overcome difficulties and adversity. However, the relationship between resilience and PTG remains controversial. Previous studies have suggested that their relationship may be positive [74], curvilinear [75], or insignificant [76], and further investigation is needed to explore the mediating and moderating factors involved. Considering the dynamic nature of resilience and PTG over time, Lyu [42] explored their trends and relationships throughout the traumatic event and discovered that individuals continue to grow in a virtuous cycle after trauma. PTG promotes psychological resilience, and PTG promotes psychological resilience. Over time, these two factors positively influence each other, contributing to the individual’s continued positive functioning during and after the adverse experience.
Psychological resilience and positive psychological qualities can assist HCWs in better emotion regulation and sensemaking, thereby promoting PTG. This finding is consistent with the model of “Posttraumatic Growth at Work” [77], confirming the importance of these individual characteristics for PTG. Therefore, enhancing psychological resilience and positive psychological qualities in medical staff can improve their growth potential in the face of traumatic events.
Coping and social support
Effective coping styles and strong social support are vital in facilitating PTG. Positive and effective coping strategies help individuals face challenges and mobilize resources from others and society to solve problems. Psychological interventions or training during or before frontline work can help HCWs maintain positive emotions, reduce attentional bias towards negative emotions, and facilitate their regulation and release, enabling them to perform their high-intensity work in a good psychological state. These interventions or training may also stimulate HCWs’ sense of mission and professional responsibility, generate positive psychological experiences, and promote growth in their front-line work [38]. Excessive attention to negative external information can trigger negative emotions, but shifting attention appropriately can help traumatized individuals detach from distress and gain new insights to reexamine and confront traumatic events. Self-motivation can enhance an individual’s self-confidence and facilitate positive psychological adjustment, prompting the traumatized person to adopt positive behaviors, solve problems, and grow. Choosing a suitable relaxation method, such as online counseling or a self-relaxation mobile app, can also help to cope effectively with pandemic stress [29].
Social support refers to the material and emotional assistance individuals receive from their social networks, including family, friends, and other socially connected individuals. Individuals can process traumatic events in a supportive environment by disclosing their internal processes to others, particularly when focusing on cognitive and emotional factors. The degree to which individuals perceive their social environment as encouraging or inhibiting plays a crucial role in the PTG process. Adequate protective materials can help HCWs better protect themselves and increase their confidence in their work, while care and support from family, friends, colleagues, and social organizations can alleviate stress and anxiety during the COVID-19 pandemic [26, 30, 39, 45, 47, 52, 53]. Good social support provides HCWs with external resources and emotional support, creating a safe atmosphere for self-expression, understanding, and acceptance [30].
Effective coping strategies and robust social support significantly impact PTG, aligning with the emphasis on social support, occupational backing, and attentive companionship in the “Posttraumatic Growth at Work” model [77]. This support can assist HCWs in modulating their emotions and provide a safe environment for sensemaking, thereby facilitating PTG. It is crucial to strengthen the training of coping abilities for medical staff and elevate social support during intervention measures.
Limitations and directions for future research
This study has several limitations that should be acknowledged. First, it only provided a descriptive analysis of the included literature and did not rigorously evaluate the studies’ quality. Second, the review focused exclusively on “posttraumatic growth” or “alternative posttraumatic growth,” omitting relevant topics such as positive posttraumatic experiences and perceived benefits. Third, only 28 of the 36 papers provided specific PTGI scores, and the data could not be integrated due to variations in PTGI versions, classification criteria, and result presentation. Additionally, most studies were cross-sectional, precluding the establishment of causal relationships. Some studies on risk factors did not control for confounding variables (work hours, COVID-19 exposure intensity, cultural background, and government policies), potentially affecting the results.
Our study’s findings point to several critical directions for future research to enhance the understanding of PTG among HCWs. Firstly, there is an urgent need for additional longitudinal studies to delve deeper into the dynamics and formation mechanisms of PTG. Such studies are essential for providing a more comprehensive understanding of how PTG evolves. Secondly, considering the global scope of the pandemic, it is crucial to understand PTG within various cultural contexts. Cultural differences in emotional experiences and expressions can significantly influence the process and potential of PTG. Therefore, future research should incorporate a cultural perspective, exploring how cultural factors impact the development and experience of PTG among healthcare professionals. This approach will not only enrich our understanding of PTG in diverse settings but also guide culturally sensitive support and intervention strategies. Lastly, future studies should focus on assessing various interventions’ efficacy to determine best practices for supporting HCWs’ psychological well-being and growth. This includes exploring how different types of support systems, both professional and societal, can facilitate PTG. The development and validation of these interventions will provide critical guidance for healthcare settings and policymakers in creating robust mechanisms to support HCWs during and after traumatic events.
Implications for practice and policy
The psychological health and PTG of medical staff are long-term concerns. To enhance the psychological resilience and PTG levels in medical staff, practice and policy should focus on the following aspects:
In terms of practical implications, we underscore the necessity of enhancing support systems tailored to the specific needs of HCWs. This involves developing interventions that address the key factors influencing PTG, such as trauma exposure and coping strategies. Such support systems could encompass resilience training programs, mental health workshops, and peer support initiatives, all designed to fortify the psychological resilience of healthcare staff. Additionally, there is a need for personalized interventions that take into account the individual psychological traits and sociodemographic factors of HCWs, thereby fostering PTG in a manner that resonates with their unique experiences and backgrounds. Furthermore, it is important to update the existing crisis response protocols to integrate measures for psychological well-being. This would ensure that HCWs’ mental health is a primary consideration during pandemics, aligning crisis responses with the psychological needs and challenges faced by these essential personnel.
Regarding policy implications, our study highlights the critical need for strategic resource allocation to enhance mental health services and support systems in healthcare settings. This is particularly crucial during public health emergencies, such as the COVID-19 pandemic, where the mental health demands of HCWs are significantly heightened. Adequate resource allocation should include not only immediate support but also long-term mental health services to address the ongoing needs of healthcare professionals. Recognizing the lasting impact of pandemic experiences on HCWs, it is imperative to develop comprehensive long-term mental health strategies. These strategies should encompass continuous support, regular mental health assessments, and adaptive interventions, ensuring that the evolving mental health needs of HCWs are met effectively. Such policies would not only provide immediate relief during crises but also contribute to the sustainable well-being and resilience of healthcare professionals in the long run.
Conclusions
This scoping review revealed that medical staff experienced moderate PTG during the COVID-19 pandemic, with notable improvements in interpersonal relationships, life philosophy, and personal competence. Key influencing factors included trauma exposure, sociodemographics, psychological traits, coping, and social support. The findings highlight the importance of addressing HCWs’ psychological well-being and resilience during and after pandemics. Further research is required to explore PTG in diverse cultural contexts, investigate the dynamic nature of PTG, and evaluate the effectiveness of targeted interventions for HCWs.
Data availability
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Abbreviations
- PTG:
-
Posttraumatic growth
- VPTG:
-
Vicarious posttraumatic growth
- PTGI:
-
Posttraumatic Growth Inventory
- PTGI-SF:
-
Short version of the posttraumatic growth inventory
- PTGI-X:
-
Expanded posttraumatic growth inventory
- COVID‑19:
-
Coronavirus disease 2019
- WHO:
-
World Health Organization
- HCWs:
-
Healthcare workers
- PRISMA‑ScR:
-
Preferred reporting items for systematic reviews and meta‑analyses extension for scoping reviews
- PTSD:
-
Posttraumatic stress disorder
- PTSS:
-
Posttraumatic stress symptoms
References
Tedeschi RG, Calhoun LG. Posttraumatic growth: conceptual foundations and empirical evidence. Psychol Inq. 2004;15(1):1–18.
Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress. 1996;9(3):455–71.
Chen X, Liu X, Shi X, Chen H, Fan F. Psychological resilience and posttraumatic growth in adolescent survivors of Earthquake: a 10-year cohort study. J Psychiatr Res. 2022;155:331–7.
Şimşek Arslan B, Özer Z, Buldukoğlu K. Posttraumatic growth in parentally bereaved children and adolescents: a systematic review. Death Stud. 2022;46(1):111–23.
Liu Z, Doege D, Thong MSY, Arndt V. The relationship between posttraumatic growth and health-related quality of life in adult cancer survivors: a systematic review. J Affect Disord. 2020;276:159–68.
Pięta M, Rzeszutek M. Posttraumatic growth and well-being among people living with HIV: a systematic review and meta-analysis in recognition of 40 years of HIV/AIDS. Qual Life Res. 2022;31(5):1269–88.
Levi-Belz Y, Krysinska K, Andriessen K. Turning personal tragedy into triumph: a systematic review and meta-analysis of studies on posttraumatic growth among suicide-loss survivors. Psychol Trauma. 2021;13(3):322–32.
Wadji DL, Oe M, Bartoli E, Martin-Soelch C, Pfaltz MC, Langevin R. How are experiences and acceptability of child maltreatment related to resilience and posttraumatic growth: a cross cultural study. Eur J Psychotraumatol. 2023;14(2):2264119.
Kangaslampi S, Peltonen K, Hall J. Posttraumatic growth and posttraumatic stress - a network analysis among Syrian and Iraqi refugees. Eur J Psychotraumatol. 2022;13(2):2117902.
Greenberg J, Tsai J, Southwick SM, Pietrzak RH. Can military trauma promote psychological growth in combat veterans? Results from the national health and resilience in veterans study. J Affect Disord. 2021;282:732–9.
Tsirimokou A, Kloess JA, Dhinse SK. Vicarious post-traumatic growth in professionals exposed to traumatogenic material: a systematic literature review. Trauma Violence Abuse. 2022:779766239.
Tabor PD. Vicarious traumatization: concept analysis. J Forensic Nurs. 2011;7(4):203–8.
Kalaitzaki AE, Tamiolaki A, Rovithis M. The healthcare professionals amidst Covid-19 pandemic: a perspective of resilience and posttraumatic growth. Asian J Psychiatr. 2020;52:102172.
Bhagwagar H. Secondary trauma, burnout and resilience among mental health professionals from India: a review of research. Asian J Psychiatr. 2022;76:103227.
World health statistics 2023. : Monitoring health for the SDGs, sustainable development goals.https://www.who.int/publications/i/item/9789240074323. Accessed 19 May 2023.
Statement on the fifteenth meeting of the ihr. (2005) emergency committee on the covid-19 pandemic.https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic. Accessed 11 May 2023.
Saragih ID, Tonapa SI, Saragih IS, Advani S, Batubara SO, Suarilah I, et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int J Nurs Stud. 2021;121:104002.
Pollock A, Campbell P, Cheyne J, Cowie J, Davis B, McCallum J, et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a Disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Database Syst Rev. 2020;11(11):D13779.
Bhardwaj A. Medical professionalism in the provision of clinical care in healthcare organizations. J Healthc Leadersh. 2022;14:183–9.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. Prisma extension for scoping reviews (prisma-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Zhang Y, Jiang WB, Lv BH, Wu Q, Li QQ, Gu RT, et al. Post-traumatic growth trajectories among frontline healthcare workers during the Covid-19 pandemic: a three-wave follow-up study in mainland China. Front Psychiatry. 2022;13:945993.
Kapur A, Rudin B, Potters L. Posttraumatic growth in radiation medicine during the Covid-19 outbreak. Adv Radiat Oncol. 2022;7(4):100975.
Yılmaz-Karaman 0G, Yastıbaş-Kaçar C. Ece 0F. Posttraumatic growth levels of healthcare workers in two periods with different intensities of COVID-19 pandemic. Psych J. 2023;12(2):297–306.
Zhang N, Bai B, Zhu J. Stress mindset, proactive coping behavior, and posttraumatic growth among health care professionals during the COVID-19 pandemic. Psychol Trauma. 2023;15(3):515–23.
Atay N, Sahin-Bayindir G, Buzlu S, Koç K, Kuyuldar Y. The relationship between posttraumatic growth and psychological resilience of nurses working at the pandemic clinics. Int J Nurs Knowl. 2023;34(3):226–35.
Jiang J, Han P, Huang X, Liu Y, Shao H, Zeng L, et al. Post-traumatic growth experience of first-line emergency nurses infected with COVID-19 during the epidemic period-A qualitative study in Shanghai, China. Front Public Health. 2022;10:1015316.
Veronese G, Mahamid FA, Bdier D. Subjective well-being, sense of coherence, and posttraumatic growth mediate the association between covid-19 stress, trauma, and burnout among Palestinian health-care providers. Am J Orthopsychiatry. 2022;92(3):291–301.
Li L, Mao M, Wang S, Yin R, Yan H, Jin Y, et al. Posttraumatic growth in Chinese nurses and general public during the COVID-19 outbreak. Psychol Health Med. 2022;27(2):301–11.
Yim JY, Kim JA. Factors influencing posttraumatic growth among nurses caring for COVID-19 patients: a path analysis. J Nurs Manag. 2022;30(6):1940–8.
Sarıalioğlu A, Çiftçi B, Yıldırım N. The transformative power of pain and posttraumatic growth in nurses with COVID-19 PCR positive. Perspect Psychiatr Care. 2022;58(4):2622–30.
Yeung NC, Wong EL, Cheung AW, Leung CS, Yeoh EK, Wong SY. Finding the positives from the COVID-19 pandemic: factors associated with posttraumatic growth among nurses in Hong Kong. Eur J Psychotraumatol. 2022;13(1):2005346.
Dahan S, Levi G, Segev R. Shared trauma during the COVID-19 pandemic: psychological effects on Israeli mental health nurses. Int J Ment Health Nurs. 2022;31(3):722–30.
Kalaitzaki A, Tamiolaki A, Tsouvelas G. From secondary traumatic stress to vicarious posttraumatic growth amid covid-19 lockdown in Greece: the role of health care workers’ coping strategies. Psychol Trauma. 2022;14(2):273–80.
Mohammed N, Lelièvre H. Lived experience of medicine nurses caring for COVID-19 patients: a quality improvement perspective. J Nurs Care Qual. 2022;37(1):35–41.
Feingold JH, Hurtado A, Feder A, Peccoralo L, Southwick SM, Ripp J, et al. Posttraumatic growth among health care workers on the frontlines of the covid-19 pandemic. J Affect Disord. 2022;296:35–40.
Chen R, Sun C, Chen JJ, Jen HJ, Kang XL, Kao CC, et al. A large-scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID-19 pandemic. Int J Ment Health Nurs. 2021;30(1):102–16.
Cui PP, Wang PP, Wang K, Ping Z, Wang P, Chen C. Post-traumatic growth and influencing factors among frontline nurses fighting against COVID-19. Occup Environ Med. 2021;78(2):129–35.
Peng X, Zhao HZ, Yang Y, Rao ZL, Hu DY, He Q. Post-traumatic growth level and its influencing factors among frontline nurses during the COVID-19 pandemic. Front Psychiatry. 2021;12:632360.
Aydin R, Bulut E. Experiences of nurses diagnosed with COVID-19 in Turkey: a qualitative study. Int Nurs Rev. 2022;69(3):294–304.
Nie T, Tian M, Liang H. Relational capital and post-traumatic growth: the role of work meaning. Int J Environ Res Public Health. 2021;18(14):7362.
Lyu Y, Yu Y, Chen S, Lu S, Ni S. Positive functioning at work during COVID-19: posttraumatic growth, resilience, and emotional exhaustion in Chinese frontline healthcare workers. Appl Psychol Health Well Being. 2021;13(4):871–86.
Moreno-Jiménez JE, Blanco-Donoso LM, Demerouti E, Belda HS, Chico-Fernández M, Moreno-Jiménez B, et al. The role of healthcare professionals’ passion in predicting secondary traumatic stress and posttraumatic growth in the face of COVID-19: a longitudinal approach. Int J Environ Res Public Health. 2021;18(9):4453.
Uziel N, Gilon E, Meyerson J, Levin L, Khehra A, Emodi-Perlman A, et al. Dental personnel in Israel, Canada, and France during the COVID-19 pandemic: attitudes, worries, emotional responses, and posttraumatic growth. Quintessence Int. 2021;52(5):444–53.
Mo Y, Tao P, Liu G, Chen L, Li G, Lu S, et al. Post-traumatic growth of nurses who faced the COVID-19 epidemic and its correlation with professional self-identity and social support. Front Psychiatry. 2021;12:562938.
DiGiovanni M, Weller I, Martin A. Pivoting in the pandemic: a qualitative study of child and adolescent psychiatrists in the times of COVID-19. Child Adolesc Psychiatry Ment Health. 2021;15(1):32.
Zhang XT, Shi SS, Qin RY, Wang L. The traumatic experience of clinical nurses during the COVID-19 pandemic: which factors are related to post-traumatic growth? Risk Manag Healthc Policy. 2021;14:2145–51.
Lee N, Lee HJ. South Korean nurses’ experiences with patient care at a COVID-19-designated hospital: growth after the frontline battle against an Infectious Disease pandemic. Int J Environ Res Public Health. 2020;17(23):9015.
Carola V, Vincenzo C, Morale C, Cecchi V, Rocco M, Nicolais G. Psychological health in intensive care unit health care workers after the covid-19 pandemic. Healthc (Basel). 2022;10(11):2201.
Li YL, Qu Q, Hu JJ, Wang YC, Huang WY. The mediating role of organizational support in the occupational resilience and post-traumatic growth of nursing staff in the prevention and control of the novel coronavirus Pneumonia epidemic. Contemp Nurses. 2022;29(02):39–42.
Cui JR, Hu LH, Huang LH, Wang H, Guan XL, Yin SY, et al. Posttraumatic growth and its related factors among nursing staff working against COVID-19 in the frontline clinical departments. Chin Nurs Manag. 2021;21(01):54–9.
Li XM, Zheng Y, Chen YP, Wu YY. Posttraumatic growth level and influencing factors of outpatient and emergency nurses under COVID-19. Chin J Med Guide. 2020;22(08):521–6.
Lv YZ, Li T, Wang QF, Liu L, Ni SG. Effect of resilience and expression suppression on the relationship between social support and posttraumatic growth among front-line medical workers in the epidemic situation of COVID-19. Chin J Clin Psychology. 2020;28(04):743–6.
Cai C, Wang X, Huang LH, Hu LH, Yi SY, Wang H, et al. A qualitative research on the experience of post-traumatic growth among nurses with covid-19. Chin Nurs Manag. 2021;21(05):712–6.
Han SJ, Chun JY, Bae HJ. Post-traumatic growth of nurses in COVID-19 designated hospitals in Korea. Int J Environ Res Public Health. 2022;20(1):56.
Prekazi L, Hajrullahu V, Bahtiri S, Kryeziu B, Hyseni B, Taganoviq B, et al. The impact of coping skills in post-traumatic growth of healthcare providers: when mental health is deteriorating due to COVID-19 pandemic. Front Psychol. 2021;12:791568.
Lv M, Tan X, Xing C, Zheng J, Han S. How family-work conflict influences post-traumatic growth among medical workers: a moderated mediation model. Front Psychol. 2021;12:743970.
Wang J, Chen Y, Wang YB, Liu XH. Revision of the posttraumatic growth inventory and testing its reliability and validity. J Nurs Sci. 2011;26(14):26–8.
Cann A, Calhoun LG, Tedeschi RG, Taku K, Vishnevsky T, Triplett KN, et al. A short form of the posttraumatic growth inventory. Anxiety Stress Coping. 2010;23(2):127–37.
Tedeschi RG, Cann A, Taku K, Senol-Durak E, Calhoun LG. The posttraumatic growth inventory: a revision integrating existential and spiritual change. J Trauma Stress. 2017;30(1):11–8.
Zoellner T, Maercker A. Posttraumatic growth in clinical psychology - a critical review and introduction of a two component model. Clin Psychol Rev. 2006;26(5):626–53.
Shakespeare-Finch J, Lurie-Beck J. A meta-analytic clarification of the relationship between posttraumatic growth and symptoms of posttraumatic distress disorder. J Anxiety Disord. 2014;28(2):223–9.
Dar IA, Iqbal N. Beyond linear evidence: the curvilinear relationship between secondary traumatic stress and vicarious posttraumatic growth among healthcare professionals. Stress Health. 2020;36(2):203–12.
Zerach G, Shalev TB. The relations between Violence exposure, posttraumatic stress symptoms, secondary traumatization, vicarious post traumatic growth and Illness attribution among psychiatric nurses. Arch Psychiatr Nurs. 2015;29(3):135–42.
Siqveland J, Nygaard E, Hussain A, Tedeschi RG, Heir T. Posttraumatic growth, depression and posttraumatic stress in relation to quality of life in tsunami survivors: a longitudinal study. Health Qual Life Outcomes. 2015;13:18.
Chen J, Zhou X, Zeng M, Wu X. Post-traumatic stress symptoms and post-traumatic growth: evidence from a longitudinal study following an Earthquake Disaster. PLoS ONE. 2015;10(6):e127241.
Ganai UJ, Sachdev S, Bhat NA, Bhushan B. Associations between posttraumatic stress symptoms and posttraumatic growth elements: a network analysis. Psychol Trauma. 2022 Dec 8.
Cao C, Wang L, Wu J, Li G, Fang R, Cao X, et al. Patterns of posttraumatic stress disorder symptoms and posttraumatic growth in an epidemiological sample of Chinese Earthquake survivors: a latent profile analysis. Front Psychol. 2018;9:1549.
Wu X, Kaminga AC, Dai W, Deng J, Wang Z, Pan X, et al. The prevalence of moderate-to-high posttraumatic growth: a systematic review and meta-analysis. J Affect Disord. 2019;243:408–15.
Cohen-Louck K. Differences in post-traumatic growth: individual quarantine, Covid-19 duration and gender. Front Psychol. 2022;13:920386.
Kucharska J. Religiosity and the psychological outcomes of trauma: a systematic review of quantitative studies. J Clin Psychol. 2020;76(1):40–58.
Lehmann C, Steele E. Going beyond positive and negative: clarifying relationships of specific religious coping styles with posttraumatic outcomes. Psycholog Relig Spiritual. 2020;12(3):345–55.
Seligman ME, Csikszentmihalyi M. Positive psychology. An introduction. Am Psychol. 2000;55(1):5–14.
Jeon G, Park S, Bernstein KS. Socio-demographic and psychological correlates of posttraumatic growth among Korean americans with a history of traumatic life experiences. Arch Psychiatr Nurs. 2017;31(3):256–62.
Kaye-Tzadok A, Davidson-Arad B. Posttraumatic growth among women survivors of childhood Sexual Abuse: its relation to cognitive strategies, posttraumatic symptoms, and resilience. Psychol Trauma. 2016;8(5):550–8.
Ogińska-Bulik N, Zadworna-Cieślak M. The role of resiliency and coping strategies in occurrence of positive changes in medical rescue workers. Int Emerg Nurs. 2018;39:40–5.
Maitlis S. Posttraumatic growth at work. Annual Rev Organizational Psychol Organizational Behav. 2020;7:395–419.
Acknowledgements
We thank the Home for Researchers editorial team (www.home-for-researchers.com) for the language editing service.
Funding
This work was supported by the General Research Project of Zhejiang Provincial Department of Education(Y202043349).
Author information
Authors and Affiliations
Contributions
Q.L. and L.W. are involved in the study conceptualization and design. Q.L. and X.Q. were involved in the search, acquisition, and management of peer-reviewed and grey literature records. Y.X., N.H., and J.G. were involved in the literature screening process. Q.L., H.L., and Y.Z. were involved in data extraction and interpretation. Q.L. prepared the initial draft of the manuscript. All authors were involved in the review and substantial revisions of the manuscript draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Q., Zhu, Y., Qi, X. et al. Posttraumatic growth of medical staff during COVID-19 pandemic: A scoping review. BMC Public Health 24, 460 (2024). https://doi.org/10.1186/s12889-023-17591-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17591-7