- Research
- Open access
- Published:
An overview of cervical cancer epidemiology and prevention in the Baltic States
BMC Public Health volume 23, Article number: 660 (2023)
Abstract
Aims
To inform future Baltic States-specific policy analyses, we aimed to provide an overview of cervical cancer epidemiology and existing prevention efforts in Estonia, Latvia and Lithuania.
Methods
A structured desk review: we compiled and summarized data on current prevention strategies, population demography and epidemiology (high risk human papillomavirus (HPV) prevalence and cervical cancer incidence and mortality over time) for each Baltic State by reviewing published literature and official guidelines, performing registry-based analyses using secondary data and having discussions with experts in each country.
Results
We observed important similarities in the three Baltic States: high burden of the disease (high incidence and mortality of cervical cancer, changes in TNM (Classification of Malignant Tumors) stage distribution towards later stage at diagnosis), high burden of high-risk HPV in general population and suboptimal implementation of the preventive strategies as low screening and HPV vaccination coverage.
Conclusions
Cervical cancer remains a substantial health problem in the region and the efforts in addressing barriers by implementing a four-step plan for elimination cervical cancer in Europe should be made. This goal is achievable through evidence-based steps in four key areas: vaccination, screening, treatment, and public awareness.
Background
For cervical cancer, effective primary and secondary prevention approaches, vaccination and screening respectively, have been successful in reducing incidence and mortality [1]. Accordingly, for the first time in history, eliminating a specific cancer from the globe is an attainable objective [2]. Improvements in cervical cancer screening programs, particularly switching to primary human papillomavirus (HPV) based testing, is considered crucial for accelerating cervical cancer elimination in studies using data from Norway [3], Australia [4], USA (United States of America) [5], and Britain [6]. Additional questions towards cervical cancer elimination are: when could elimination be achieved, and how is this timeline modified by the secondary prevention strategies selected by different countries? Depending on national cervical cancer prevention policies large variations are expected in terms of when cervical cancer will be eliminated. Mathematical models predict Australia to be on-track to eliminate cervical cancer by 2028 [4] and USA between 2038 and 2046 [5], while many countries without existing screening programs are unlikely to be cervical cancer-free this century. Detailed knowledge of the epidemiology of a disease, and prevention strategies implemented, contribute to fill the knowledge gaps.
In Europe, cervical cancer ranks as the 9th most frequent cancer among women and the 2nd most common for cancer deaths in women aged 15 to 44 years [7].. Europe is characterised by considerable disparities in incidence and mortality of cervical cancer. The Baltic States are among those European countries with the highest incidence and mortality from cervical cancer [8, 9].
The aim of this article is to provide an overview of the epidemiology of cervical cancer as well as ongoing prevention strategies in the Baltic States and to outline the steps to accelerate the trend towards cervical cancer elimination.
Methods
A structured desk review was conducted with the documents related to cervical cancer prevention policies, protocols, practice guidelines, evaluation reports, and others, issued/published by the countries’ relevant authorities. This was complemented with other pertinent documents (including peer-reviewed journal publications) identified by the working group of experts. This review was undertaken by national experts from Estonia, Latvia and Lithuania. We selected the key performance indicators - screening intensity, screening test performance, diagnostic assessment, treatment, and post-treatment follow-up of screening and vaccination programmes [10].
The most recent data regarding cervical cancer epidemiology and prevention measures in the Baltic States are presented. The data on number of cervical cancer (International Classification of Diseases tenth edition [ICD-10] code C53) cases and deaths for the period of 1990–2018 originated from the population-based cancer and death registries in Latvia, Estonia, and Lithuania. For each country, data on the size of the female population at the screening age, size of female birth cohort, and the life expectancy for women were retrieved [11,12,13].
We summarized the current status of cervical cancer prevention in these countries in order to identify areas of consistent findings, gaps in practice, and necessary next steps for research and public health practice.
Statistical analysis
The age-standardized incidence (ASIRs) and mortality (AMIRs) rates per 100,000 were computed (using World population) [14]. The 95% confidence intervals (CIs) were computed by assuming Poisson distribution for incident and mortality counts. Joinpoint regression program [15] was used to model the rates and calculate the estimated annual percent change (APC) with 95% CI. We computed the average age at cervical cancer diagnosis and death as the weighted mean age using the mid-age of each 5-year age group for the period of 2014–2018 for Estonia and Latvia and for the period of 2014–2015 for Lithuania. Union for International Cancer Control version 7 of the TNM classification for malignant tumours was used to categorise stage. The TNM stage was obtained from the cancer registry and was available for cases diagnosed from 2005 and forward. The distribution by TNM stage is presented for the time periods 2005–2009 and 2014–2018 (Lithuania 2014–2015).
Results
Population demography
In 2020 the proportion of female population in three Baltic States was similar, the total population in Estonia was 1,331,057 (52.6% women), in Latvia 1,901,548 (53.9% women), and in Lithuania 2,794,700 (53.7% women) [16]. The female population life expectancy at birth has increased to over 80 years over the last three decades. The largest increase from 1990 to 2019 was reported in Estonia from 74.8 to 82.8, then Latvia from 74.6 to 79.9 and Lithuania from 76.2 to 81.0 [17].
In 2019, the size of the female screening population ranged from 233,226 in Estonia (aged 30–55 years) to 636,528 in Lithuania (aged 29–59 years), and annual female birth cohorts ranged from 6,734 in Estonia to 14,672 in Lithuania (10,197 in Latvia) (Table 1).
HPV prevalence
A subnational study conducted in 2006 in Estonia reported an overall prevalence of 38.6% for HPV DNA in a random sampling of women with unknown cytology aged 18–35 years. High and low risk HPV prevalence was 21.3% (95% CI 16.4–26.8) and 10.1% (95% CI 7.2–14.3) respectively. HPV 16 was detected most frequently (6.4%; 95% CI 4.0-9.8%) followed by HPV 53 (4.3%; 95% CI 2.3–7.2) and HPV 66 (2.8%; 95% CI 1.3–5.2) [18].
A study from 2007 including data from Latvia reported a high-risk HPV (hrHPV) DNA (deoxyribonucleic acid) prevalence of 26.2% (9 hrHPV types tested) with a convenient sampling from three sources: women aged 15–85 attending screening, gynecologist consultation, or a sexually transmitted disease clinic. HPV 16 was the most common type (16.0%) detected. The prevalence of hrHPV when excluding women with abnormal cervical cytology findings was 21.5% [19].
From Lithuania data are available from a two region gynaecology clinic attendees-based samples from mid 2000s, that yielded hrHPV test positivity among women aged 18–50 of 25.0% (13 types hrHPV tested) [20].
In Latvia, the prevalence of HPV 16/18 among women with low-grade squamous intraepithelial lesions / cervical intraepithelial neoplasia grade 1 (LSIL/CIN-1) is the highest among the Baltic States at 35.1%, while Estonia is slightly lower at 30.6% and Lithuania differing significantly at 6.7% [21].
HPV in cervical precancerous lesions and cervical cancer
In Lithuania, 74.2% women with CIN2/3 and 85.6% of women with cervical cancer, were hrHPV positive. HPV 16 was the most prevalent subtype, detected in 50% of cervical cancers and CIN 2/3 cases, followed by ~ 10% prevalence of HPV 18 and HPV 33 in both disease groups [22]. Estonian data is closely mirroring these results – with prevalence of 55%, 12% and 8% for HPV 16, 33 and 31 respectively among women with high grade cervical lesions [23].
According to the study from Latvia by Silins et al. (2004), the most common HPV DNA type found in cervical samples of the cervical cancer patients was HPV 16 (60.6%), followed by HPV 18 (9.0%), HPV 31 (5.4%), HPV 45 (3.2%), and HPV33 (2.7%). Overall, 82.8% (183/ 221) of examined samples were HPV-positive [24, 25].
Cervical cancer - primary prevention
There are organized population-based HPV vaccination programmes in all three Baltic States. Vaccination of the target population is free of charge and includes 12-18-year-old girls in Latvia, 12-14-year-old girls in Estonia, and 11-year-old girls in Lithuania. School-based vaccination is performed in Estonia and Lithuania, but in Latvia vaccination is provided by general practitioners (Table 1).
Cervical cancer - secondary prevention
In the three countries opportunistic and organised screening coexist. For example, in Estonia, about 90% of all Pap tests (Papanicolaou cytological staining) are performed in Estonia every year outside of organized screening [26]. Organized nation-wide cervical cytology-based screening programmes in the Baltic States have been in operation for over 10 years (Table 1).
Until 2020, cytology was the primary screening test in all three Baltic States. Pap test and Bethesda classification, recommended by the European guidelines [27], used in Estonia and Lithuania prior to this, and Giemsa stain with Leishman modification test (historical tradition from former Soviet Union cytology practice) in Latvia [28]. In 2021 Latvia switched to liquid-based cytology using Bethesda classification as a primary screening test, and Estonia to HPV DNA test.
In 2006, a nation-wide programme of the screening with the five-year interval was initiated and organized via screening cabinets in clinics that participated in the programme with specially trained midwives taking Pap test [29]. The National Health Insurance Fund under the Ministry of Social Affairs finances the programme. Since 2015, the Registry of Cancer Screening is responsible for sending invitations and monitoring the process. Women are invited for organised screening using individual invitation letters sent by e-mail, by post, or via the media information campaigns (the exact methodology of invitation differs by year). In January 2021 Estonia implemented new guidelines recommending primary HPV DNA testing for a wider age range (30 to 65 years) of women with a five-year interval [30].
In Latvia, organized cervical cancer screening started in 2009 for women aged 25–70 years using cytology test (a modified Leishman Giemsa staining). All eligible women are invited by the National Health Service to attend a screening appointment every 3 years. Invitations letters are mailed to women’s declared addresses. Screening tests are usually performed at a gynaecological clinic, general practitioners rarely take Pap smears and nurses or midwives are not involved. Although primary care practitioners are not actively involved in the screening programme, they can monitor whether their female patients have attended screening. NHS collects results of the screening tests, but ongoing follow up and monitoring of the system is not provided.
The Lithuanian National Cervical Cancer Screening Programme was launched in 2004, which is financed by the National Health Insurance Fund under the Ministry of Health of Lithuania offering a free Pap smear test every 3 years to all women aged 25–60 years.
Primary health care practitioners are responsible for inviting and screening women. Usually, personal invitations are not sent out by mail and primary practitioners (GP) tend to rely on informing women about the screening when they attend their primary health care centre [31, 32]. Thou, programme still carries opportunistic features as it is strongly dependent on the frequency of visits to the GP and the activity of the GP in providing information about screening [33]. Data on the exact coverage of screened women are currently not available. Research projects testing the efficacy of personal invitation letters conducted in 2011 and 2014 in Lithuania yielded response rates (coverage) ranging from 22% [31] to 25% [32].
Cervical cancer screening registries are established in Latvia (2009), and Estonia (2015) [34] but not in Lithuania [35]. All three countries lack comprehensive screening test quality control systems.
Cervical cancer incidence
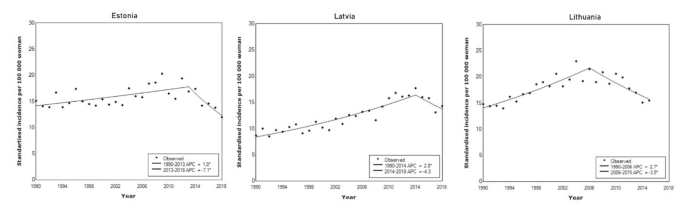
ASIRs are shown in Fig. 1 for women of all ages (0+) from the beginning of the observation period in 1990 until the end of the observation in 2018 (or in the last available year before 2018). During the period of 2014–2018, the average ASIR for cervical cancer in the three Baltic States were as follows − 14.4 per 100,000 women in Estonia, 15.4 per 100,000 women in Latvia, and 15.5 per 100,000 women in Lithuania (2014–2015). In all countries, ASIR increased starting from 1990 to peak between 2006 and 2014. In Estonia, ASIR increased from 1990 to 2013 by APC = 1.0% (95% CI 0.4–1.6) with the highest cervical cancer ASIR of 20.3 and 19.4 per 100,000 women in 2009 and 2012. From 1990 to 2014, Latvia witnessed a steep increase of cervical cancer incidence (APC = 2.8, 95% CI 2.3–3.4) with the peak ASIR of 17.7 per 100,000 women in 2014. SIR in Lithuania increased from 1990 to 2006 by APC = 2.7 (95% CI 2.0–3.5), with the highest rates observed in 2004 (23.0 per 100,000 women) and 2006 (21.5 per 100,000 women).
By the end of observation period, we had seen a decrease in ASIR in all three countries: by APC = -3.5 (95% CI − 1.8 – -5.2) in Lithuania, by APC = -4.3 (95% CI − 11.5–3.4) in Latvia, and by APC = -7.1 (95% CI -1.7 – -12.2) in Estonia (Fig. 1; Table 1).
For the period of 2014–2018 average age-specific cervical cancer incidence rates were estimated (Fig. 2). In Estonia, the highest rates were observed for women aged 50–54 years (41.4 per 100,000 women) and 55–59 years (38.2 per 100,000 women). In Latvia, the highest rate occurred with women aged 45–49 years at 46.5 cases per 100,000 women. In Lithuania, highest age-specific incidence rates were observed in age groups 45–49 years (43.0 per 100,000 women), 50–54 years (49.0 per 100,000 women), and 55–59 years (44.5 per 100,000 women).
The cumulative incidence of cervical cancer by age 75 was 1.4 in Estonia, 1.5 in Latvia, and 1.5 in Lithuania. The one-year relative survival ranged from 74.6% in Latvia to 86% in Estonia, and five-year relative survival ranged from 51.0% in Latvia to 67% in Estonia (Table 1).
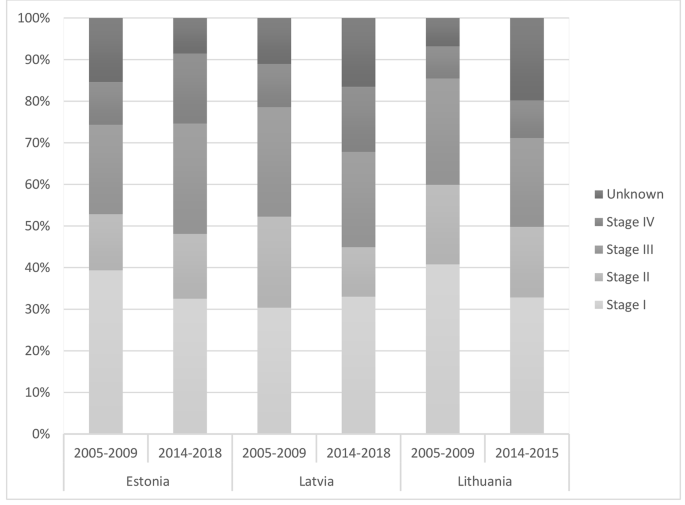
Cervical cancer stage distribution at the time of diagnosis
Across the countries and years, about one third of cervical cancer cases have been diagnosed at stage I. In Estonia and Lithuania, TNM stage distribution shifted towards later stages at diagnosis from 2005 to 2009 to 2014–2018. The proportion of stage I cases decreased from 39.3 to 32.5% while stage IV cases increased from 10.3 to 16.9% in Estonia. In Lithuania stage I cases went from 40.8 to 32.8% and stage IV cases increased from 7.7 to 9.1% (Fig. 3).
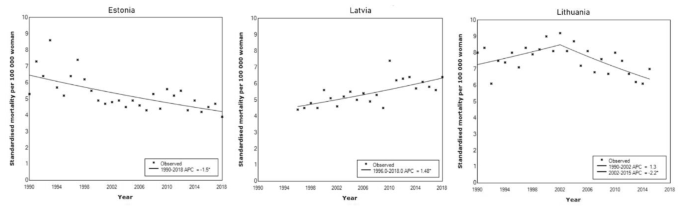
Cervical cancer mortality
In Estonia, the AMIRs declined throughout the period under analysis by APC= -1.5 (95% CI -0.9 – -2.1). In 2018, cervical cancer AMIR was 3.9 per 100,000 women. In contrast, in Latvia, the AMIR increased (APC= 1.5, 95% CI 0.8–2.1), and in 2018 cervical cancer AMIR was 6.4 per 100,000. In Lithuania, age-standardised mortality was stable until 2002 (APC = 1.3, 95% CI -0.2–2.8), and declined thereafter (APC= -2.2, 95% CI -0.8 – -3.5) (Fig. 4).
Discussion
We have provided a comprehensive overview of the trends in cervical cancer incidence and mortality, and an update of the cervical cancer prevention efforts in the Baltic States. In parallel to the increase in life expectancy over the last three decades, cervical cancer remains a substantial health problem in the region. We observed important similarities among the three countries: high burden of the disease (high incidence and mortality of cervical cancer, changes in TNM stage distribution towards later stage at diagnosis (in Lithuania and Estonia), high burden of hrHPV in general population and suboptimal implementation of the preventive strategies (low screening and HPV vaccination coverage).
Disease burden
Among general population women, the prevalence of hrHPV in Estonia and Lithuania is higher than that reported from central and western European countries and is comparable to former Soviet Union countries [18, 20, 25, 36, 37]. This tendency might be explained by the influence of the primary prevention (insufficient sexual education at schools as well as the limited effect of HPV vaccination – it has been introduced in 2018 in Estonia for girls aged 12–14 years (12 years since 2020) and in 2016 in Lithuania for girls aged 11 years, but the coverage seems to be insufficient (31.3% in Estonia in 2019, no data for Lithuania), cultural and regional relations from Soviet Union times but also can be attributed to the differences in study design and use of different HPV testing methods [38].
In comparison to neighbouring Scandinavian countries, cervical cancer incidence in the Baltic States is higher and the decline of the incidence rate has been delayed for about 50 years. Over two thirds of the period of observation, the cervical cancer incidence increased, and has only started a downward trend in more recent years. The highest age-specific incidence is also similar in Baltic States – among women aged 50–59 years, with Latvia in the slightly younger age group of 45–49 years. A slight peak is also observed after the age of 70.
Cervical cancer mortality in the Baltic countries exceeds that in neighbouring Scandinavian or Western European countries by more than two times [39]. There are some differences in cervical cancer mortality trends in the Baltic States. While the absolute mortality rates differ, in Estonia and Lithuania the mortality is declining. In Latvia, it is gradually increasing. Whether or not the decline in mortality can be attributed to screening effect is debatable. A very worrisome sign is shifting the cancer into later stages at cervical cancer diagnosis in Estonia and Lithuania [40].
Cervical cancer prevention
Data from other countries have shown that vaccination effectively reduces the prevalence of HPV, cervical high-grade precancerous lesions, and cancer [41, 42].
Vaccination against HPV has been introduced among teenage girls in all Baltic States, but the vaccination coverage is suboptimal. Studies have shown, that the main barriers to HPV vaccination are the lack of HPV awareness among the general public, lack of provider recommendation, concerns about HPV vaccination [43]. Young adults need parental consent for the vaccination and the acceptance of the HPV vaccine is highly dependent on the knowledge, perceptions, and approval of their parents. ‘Fake news’ about vaccination safety generally and HPV vaccination specifically has been associated with rapid fall in uptake in Europe [44]. There is a clear need to improve public knowledge about the value and the safety of vaccination. The possible solutions are increasing health literacy, professional awareness of HPV and the dissemination of emotive stories of patient advocates [45].
While the organised cervical cancer screening programmes in the Baltic States differ in some relevant details (target age groups, screening interval), the underlying principles (being population-based with repeated screening episodes over an extended period) and problems, barriers (low coverage, inadequately working screening test, lacking / inconsistent quality control system) are universal. Screening at the population level every three to five years can reduce cervical cancer incidence up to 80% [27]. Low attendance and lack of assured high-quality of screening programmes in all Baltic States potentially contribute to high cervical cancer incidence, and mortality. Several factors are recognized to impact screening attendance rate in the Baltic States, including personal (fear to give a Pap-smear, did not like the physician who took the sample, lack of time) and organizational (long waiting list for an appointment, distant location of the clinic [46, 47]. Local research has postulated that besides inadequate screening uptake, also the insufficient quality of the Pap-smear based screening program as drives behind the failure of cervical cancer prevention [48]. The introduction of primary HPV screening is strongly recommended to decrease cervical cancer incidence [49]. HPV testing has several advantages as a primary screening strategy, including equivalent or higher sensitivity than Pap-smears, ability to predict women at high risk for future disease, lower technician skill level needed when compared to cytology, and having the potential for self-collection [50].
Special efforts are needed to increase screening attendance in general and among high-risk women. Potentially, multiple components culturally tailored cervical cancer screening intervention combining education, and navigation, in addition to no-cost screening for all women, are needed to significantly increase cervical cancer screening uptake and to alleviate cervical cancer health disparities.
Importantly, we were unable to locate data on screening test performance, diagnostic assessment, treatment efficiency, and post-treatment follow-up. Scarcity of these data potentially indicates on weakness of organised screening programmes in Baltic States. Quality management processes distinguish organised screening programmes from opportunistic screening. Quality is an integral part of screening programmes, and proactive approach to quality improvement is required to achieve the vision, strategic outcomes [51].
No studies have been conducted to determine the practice of cervical cancer prevention and adherence to cervical cancer screening and treatment guidelines among healthcare professionals in Baltic countries within the last 10 years. There is a lack of information in regard to the knowledge on barriers to comply. According to a qualitative study conducted by Estonian health insurance fund, the delivery of cervical cancer prevention programs can vary among screening and treatment providers. The focus group participants have indicated that education of health professionals on cervical cancer preventative clinical practices should be continuous and regular [52].
Cervical cancer elimination depends strongly on contextual factors. The evidence is there - through cost-effective, evidence-based interventions, including improving public and professional awareness and education about HPV, universal HPV vaccination, high level uptake of the screening and treatment of precancerous lesions according to best practice guidelines, and assuring access to diagnosis and treatment of invasive cancers, cervical cancer as a public health problem is amenable for elimination. We see the most important factors that should be acted upon in Baltic States: (i) a political decision to accelerate activities; (ii) ownership and the performance of the national screening programs; and (iii) their adaptability to new interventions.
Conclusions
High cervical cancer incidence and mortality urge not only the use of well-validated methods in screening but also the introduction of systematic monitoring, evaluation, and quality assurance in the programme and other related services. To do this, a collaboration between cervical cancer screening programmes in other countries is required. The goal of cervical cancer free future in Baltic States could be achieved through realistic investment and evidence-based steps improving vaccination and screening coverage, public and professional awareness and treatment outcomes.
Data availability
The datasets generated and analysed during the current study are not publicly available due to the fact that no primary data are used in the study; only anonymized secondary data from population-based registries are used (aggregated data), but they are available from the corresponding author on reasonable request.
Abbreviations
- AMIR:
-
age-standardized mortality rate
- APC:
-
annual percent change
- ASIR:
-
age-standardized incidence rate
- CI:
-
confidence interval
- CIN-1:
-
cervical intraepithelial neoplasia grade 1
- CIN-2/3:
-
cervical intraepithelial neoplasia grades 2/3
- DNA:
-
deoxyribonucleic acid
- EEA:
-
European Economic Area
- GP:
-
primary practitioner
- HPV:
-
high risk human papillomavirus
- hrHPV:
-
high-risk HPV
- ICD-10:
-
International Classification of Diseases tenth edition
- LSIL:
-
low-grade squamous intraepithelial lesions
- Pap test:
-
Papanicolaou cytological staining
- TNM:
-
Classification of Malignant Tumors
- USA:
-
United States of America
References
Vaccarella S, Lortet-Tieulent J, Plummer M, et al. Worldwide trends in cervical cancer incidence: impact of screening against changes in disease risk factors. Eur J Cancer. 2013;49:3262–73.
World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem. https://www.who.int/publications/i/item/9789240014107 (2020, accessed 6th April 2022)
Portnoy A, Pedersen K, Trogstad L, et al. Impact and cost-effectiveness of strategies to accelerate cervical cancer elimination: a model-based analysis. Prev Med. 2021;144:106276.
Hall MT, Simms KT, Lew JB, et al. The projected timeframe until cervical cancer elimination in Australia: a modelling study. The Lancet Public health. 2019;4:19–27.
Burger EA, Smith MA, Killen J, et al. Projected time to elimination of cervical cancer in the USA: a comparative modelling study. Lancet Public Health. 2020;5:213–22.
Castanon A, Rebolj M, Sasieni P. Is a delay in the introduction of human papillomavirus-based cervical screening affordable? J Med Screen. 2019;26:44–9.
Bruni L, Albero G, Serrano B et al. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in the World.Summary Report October2021
Wojtyla C, Ciebiera M, Kowalczyk D, et al. Cervical Cancer mortality in East-Central European Countries. Int J Environ Res Public Health. 2020;17:4639.
Arbyn M, Weiderpass E, Bruni L, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. The Lancet Global health. 2020;8:191–203.
Publication Office of the European Union. European guidelines for quality assurance in cervical cancer screening. https://op.europa.eu/en/publication-detail/-/publication/a41a4c40-0626-4556-af5b-2619dd1d5ddc (accessed 6th April 2022)
Central Statistical Bureau of Latvia. Population number and characteristics, https://data.stat.gov.lv/pxweb/en/OSP_PUB/START__POP__IR/ (2021, accessed 6th January 2021)
Statistics Estonia. https://andmed.stat.ee/en/stat (2021, accessed 12 January 2021)
Statistics Lithuania. https://osp.stat.gov.lt/lietuvos-gyventojai-2020/mirtingumas/vidutine-tiketina-gyvenimo-trukme (2021, accessed 12 January 2021)
Bray F, Colombet M, Mery L, et al. Cancer incidence in five continents, vol. XI (electronic version). Lyon: International Agency for Research on Cancer; 2017.
National Cancer Institute. Joinpoint trend analysis software. https://surveillance.cancer.gov/joinpoint/ (2022, accessed December 1st, 2021)
The Wolrd Bank. Population total Estonia, Latvia, Lithuania. https://data.worldbank.org/indicator/SP.POP.TOTL?locations=EE-LV-LT%20Female:%20https://data.worldbank.org/indicator/SP.POP.TOTL.FE.IN?locations=EE-LV-LT%20 (2022, accessed 18 March 2022)
The World Bank. Life expectancy at birth. https://data.worldbank.org/indicator/SP.DYN.LE00.FE.IN?locations=EELV-LT(2022, accessed 18 March 2022)
Uusküla A, Kals M, Kosenkranius L, et al. Population-based type-specific prevalence of high-risk human papillomavirus infection in Estonia. BMC Infect Dis. 2010;10:63.
Kulmala SM, Shabalova IP, Petrovitchev N, et al. Prevalence of the most common high-risk HPV genotypes among women in three new independent states of the former Soviet Union. J Med Virol. 2007;79:771–81.
Kliucinskas M, Nadisauskiene RJ, Minkauskiene M. Prevalence and risk factors of HPV infection among high-risk rural and urban lithuanian women. Gynecol Obstet Invest. 2006;62:173–80.
HPV Information Centre. https://hpvcentre.net/datastatistics.php (2021, accessed 12 Janury 2021)
Gudleviciene Z, Kanopiene D, Didziapetriene J, et al. Differences on the prevalence of cervical HPV between Lithuania and Belarus. Cent Eur J Med. 2014;9:285–91.
Padrik L, Raud T, Kriisa L et al. HPV DNA prevalence in Estonian women with high-grade Lesions. European Federation for Colposcopy. Berlin 27–29 May 2010
Silins I, Wang X, Tadesse A, et al. A population-based study of cervical carcinoma and HPV infection in Latvia. Gynecol Oncol. 2004;93:484–92.
Poljak M, Seme K, Maver PJ, et al. Human papillomavirus prevalence and Type-Distribution, Cervical Cancer Screening Practices and current status of vaccination implementation in Central and Eastern Europe. Vaccine. 2013;31:59–70.
Koreinik L, EMAKAKAELAVÄHI SÕELUURINGUS OSALEMIST MÕJUTAVAD TEGURID, EESTIS. (2019) https://dspace.ut.ee/handle/10062/66725 (accessed 07 April 2022)
Arbyn M, Anttila A, Jordan J et al. European Guidelines for Quality Assurance in Cervical Cancer Screening. Second edition. IARC, 2008
Viberga I, Engele L, Baili P. Past, present and future of the cervical cancer screening in Latvia. Tumori. 2010;96:529–37.
Partanen V, Antilla A, Heinävaara S et al. NordScreen: Performance indicators on cancer screening in the Nordic countries, https://nordscreen.org/wp-content/uploads/2017/07/cervix-fact-sheet-estonia-2017.pdf (2019, accessed 01.09 2020)
National Health Insurance Fund. Screenings for women https://haigekassa.ee/soeluuring (2022, accessed 31 January 2022)
Kurtinaitienė R, Rimienė J, Labanauskaitė I, et al. Increasing attendance in a cervical cancer screening programme by personal invitation: experience of a lithuanian primary health care centre. Acta Med Lituanica. 2016;23:180–4.
Paulauskiene J, Ivanauskiene R, Skrodeniene E, Petkeviciene J. Organised Versus Opportunistic Cervical Cancer Screening in Urban and Rural Regions of Lithuania. Medicina. 2019;55(9):570.
Maver PJ, Seme K, Korać T et al. Cervical cancer screening practices in central and eastern Europe in 2012. Acta dermatovenerologica Alpina, Pannonica, et Adriatica 2013; 22: 7–19
National institute for health development.Cancer screening registries, https://tai.ee/et/tegevused/registrid/vahi-soeluuringute-register (2021, accessed 13 January 2021)
Vale DB, Anttila A, Ponti A, et al. Invitation strategies and coverage in the population-based cancer screening programmes in the European Union. Eur J Cancer Prev. 2019;28:131–40.
Rogovskaya SI, Shabalova IP, Mikheeva IV, et al. Human papillomavirus prevalence and type-distribution, cervical cancer screening practices and current status of vaccination implementation in Russian Federation, the western countries of the former Soviet Union, Caucasus region and Central Asia. Vaccine. 2013;7:46–58.
Bosch FX, Broker TR, Forman D, et al. Comprehensive control of human papillomavirus infections and related diseases. Vaccine. 2013;7:1–31.
Wang W, Kothari S, Baay M, et al. Real-world impact and effectiveness assessment of the quadrivalent HPV vaccine: a systematic review of study designs and data sources. Expert Rev Vaccines. 2022;21:227–40.
European Cancer Information System. Series of Cancer Fact Sheets EU 27 countries. https://ecis.jrc.ec.europa.eu/factsheets.php (2020, accessed 12 January 2021)
Everatt R, Intaite B. Trends in cervical cancer mortality rates in Lithuania, 1987–2016. Cancer Epidemiol. 2018;57:85–9.
Drolet M, Bénard É, Pérez N, et al. Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: updated systematic review and meta-analysis. Lancet. 2019;394:497–509.
Lei J, Ploner A, Elfström KM, et al. HPV Vaccination and the risk of Invasive Cervical Cancer. N Engl J Med. 2020;383:1340–8.
Cartmell KB, Young-Pierce J, McGue S, et al. Barriers, facilitators, and potential strategies for increasing HPV vaccination: a statewide assessment to inform action. Papillomavirus Res. 2018;5:21–31.
Suppli CH, Hansen ND, Rasmussen M, et al. Decline in HPV-vaccination uptake in Denmark – the association between HPV-related media coverage and HPV-vaccination. BMC Public Health. 2018;18:1360.
European Cancer Organisation. A four step plan for eliminating HPV cancers in Europe. https://www.europeancancer.org/resources/159:viral-protection-achieving-the-possible-a-four-step-plan-for-eliminating-hpv-cancers-in-europe.html (2020, accessed 1 February 2022)
Zodzika J, Krumina K, Jermakova I, et al. Post-reproductive aged women: a lost generation in the cervical cancer screening programme. Eur J Contracept Reprod Health Care. 2021;26:23–8.
Kivistik A, Lang K, Baili P, et al. Women’s knowledge about cervical cancer risk factors, screening, and reasons for non-participation in cervical cancer screening programme in Estonia. BMC Womens Health. 2011;11:43.
Ojamaa K, Innos K, Baburin A, et al. Trends in cervical cancer incidence and survival in Estonia from 1995 to 2014. BMC Cancer. 2018;18:1075.
Anttila A, Lönnberg S, Ponti A, et al. Towards better implementation of cancer screening in Europe through improved monitoring and evaluation and greater engagement of cancer registries. Eur J Cancer. 2015;51:241–51.
Mandelblatt JS, Lawrence WF, Womack SM, et al. Benefits and costs of using HPV testing to screen for cervical cancer. JAMA. 2002;287(18):2372–81.
World Health Organization. Screening programmes: a short guide. Increase effectiveness, maximize benefits and minimize harms. https://www.euro.who.int/en/publications/abstracts/screening-programmes-a-short-guide.-increase-effectiveness,-maximize-benefits-and-minimize-harm-2020 (2020, accessed 1 March 2022)
Ental H, Aavik HM, Lubi K, Plešs N. Estonian Cervical Cancer Screening – an opportunity that should not be missed. Road project report 2021. Estonian health insurance fund. 2021.
European Cancer Registry. Survival of cancer patients in Europe. http://www.eurocare.it/ (2021, accessed 12 January 2021)
Acknowledgements
Not applicable.
Funding
This work was supported through grant EMP416 from the EEA (European Economic Area) and Norway Grants.
Author information
Authors and Affiliations
Contributions
UK elaborated the conceptual framework of the article, carried out the calculations, drafted the text, AT elaborated the conceptual framework of the article, requested the data from national registries, drafted the text, KP elaborated the conceptual framework of the article, drafted the text, AKU requested the data from national registries, drafted and reviewed the text, JZ elaborated the conceptual framework of the article, drafted the text, MS requested the data from national registries, reviewed the text, NB elaborated the conceptual framework of the article, reviewed the text, MN elaborated the conceptual framework of the article, reviewed the text, AU elaborated the conceptual framework of the article, drafted and reviewed the text.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Consent to participate - not applicable as no primary data are used in the study; only anonymized secondary data from population-based registries are used (aggregated data). Ethics approval - approved by Research Ethics Committee of the University of Tartu (protocols 300/T-17 20.01.2020, 332/M-7 21.12.2020), Estonian Committee on Bioethics and Human Research (protocol 1.1–12/660, 14.01.2021), Research Ethics Committee of Riga Stradins University (decision No 6 − 1/07/33, 25.06.2020).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kojalo, U., Tisler, A., Parna, K. et al. An overview of cervical cancer epidemiology and prevention in the Baltic States. BMC Public Health 23, 660 (2023). https://doi.org/10.1186/s12889-023-15524-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15524-y