- Research
- Open access
- Published:
Public health emergency preparedness for infectious disease emergencies: a scoping review of recent evidence
BMC Public Health volume 23, Article number: 420 (2023)
Abstract
Background
The COVID-19 pandemic continues to demonstrate the risks and profound health impacts that result from infectious disease emergencies. Emergency preparedness has been defined as the knowledge, capacity and organizational systems that governments, response and recovery organizations, communities and individuals develop to anticipate, respond to, or recover from emergencies. This scoping review explored recent literature on priority areas and indicators for public health emergency preparedness (PHEP) with a focus on infectious disease emergencies.
Methods
Using scoping review methodology, a comprehensive search was conducted for indexed and grey literature with a focus on records published from 2017 to 2020 onward, respectively. Records were included if they: (a) described PHEP, (b) focused on an infectious emergency, and (c) were published in an Organization for Economic Co-operation and Development country. An evidence-based all-hazards Resilience Framework for PHEP consisting of 11 elements was used as a reference point to identify additional areas of preparedness that have emerged in recent publications. The findings were analyzed deductively and summarized thematically.
Results
The included publications largely aligned with the 11 elements of the all-hazards Resilience Framework for PHEP. In particular, the elements related to collaborative networks, community engagement, risk analysis and communication were frequently observed across the publications included in this review. Ten emergent themes were identified that expand on the Resilience Framework for PHEP specific to infectious diseases. Planning to mitigate inequities was a key finding of this review, it was the most frequently identified emergent theme. Additional emergent themes were: research and evidence-informed decision making, building vaccination capacity, building laboratory and diagnostic system capacity, building infection prevention and control capacity, financial investment in infrastructure, health system capacity, climate and environmental health, public health legislation and phases of preparedness.
Conclusion
The themes from this review contribute to the evolving understanding of critical public health emergency preparedness actions. The themes expand on the 11 elements outlined in the Resilience Framework for PHEP, specifically relevant to pandemics and infectious disease emergencies. Further research will be important to validate these findings, and expand understanding of how refinements to PHEP frameworks and indicators can support public health practice.
Background
The Coronavirus Disease 2019 (COVID-19) pandemic is responsible for millions of deaths globally [1, 2], and continues to demonstrate the risks and profound health impacts that result from infectious disease emergencies. While disasters and emergencies were known to have inequitable impacts across populations prior to the COVID-19 pandemic [3, 4], the disparities in COVID-19 outcomes have been grave [5,6,7]. Since the start of the pandemic, there have been demonstrable inequities in COVID-19 morbidity and mortality in marginalized communities such as racialized, low-income and Indigenous communities in Canada, as well as inequitable impacts of implementing and removing public health measures at different time periods throughout the pandemic [7,8,9]. Ecological impacts of climate change, population growth trends, and increasing population density are amongst the factors increasing global risks for the emergence of novel infectious diseases [10,11,12]. It is crucial to ensure a continued review and reflection on emergency preparedness to assess ongoing risks, to reduce morbidity and mortality, and to mitigate the inequitable impacts of infectious disease emergencies and response measures, which is the focus of this review.
The World Health Organization (WHO) Strategic Framework (2017) has defined emergency preparedness as the knowledge, capacity and organizational systems that governments, response and recovery organizations, communities, and individuals develop to anticipate, respond to, or recover from emergencies [13]. Operationally, emergency preparedness involves specific actions, funding, partnerships and political commitment to be sustainable [13]. Investing in and implementing priority actions requires an understanding of these characteristics and elements of preparedness, and can benefit from metrics to describe, assess, and report on change over time. Following the 2003 Severe Acute Respiratory Syndrome (SARS-CoV-1) outbreak and the 2009 H1N1 influenza pandemic, multiple authors in different countries noted a lack of evidence to inform definitions and metrics for public health emergency preparedness (PHEP) [14,15,16]. To address this knowledge gap in defining and measuring PHEP for the Canadian context and relevant to other jurisdictions of similar context, a Canadian-based research team, including several authors of this paper, explored PHEP for infectious and non-infectious emergencies, and developed an evidence-based, all-hazards Resilience Framework for PHEP and corresponding indicators to advance performance measurement for the field [17,18,19].
Through the previous research, performance measurement for PHEP was advanced by articulating the essential elements of PHEP and identifying indicators corresponding to the elements relevant to the context of Canada and other similar jurisdictions [17,18,19]. While the research preceded the COVID-19 pandemic, it represented a novel contribution to the field to provide evidence-based support for defining and measuring preparedness. The framework consists of 11 elements: governance and leadership (cross-cutting), planning process, collaborative networks, community engagement, risk analysis, surveillance and monitoring, practice and experience, resources, workforce capacity, communication, and learning and evaluation. A visual representation of the Resilience Framework for PHEP along with a detailed description of the 11 elements is summarized in additional file 2 [17]. The set of 67 PHEP indicators correspond with the framework’s elements and were developed based on existing indicators of PHEP from the literature, and refined and augmented by an expert panel using a structured consensus method [19]. Ethics and values were identified in this research as core to all elements of PHEP rather than as a specific element with corresponding indicators; thus, are depicted as the framework centre. Examples of ethics and values identified in the research included transparency, reciprocity, trust and equity [18]. The framework and indicators can be used by local or regional public health agencies to assess readiness and measure improvement in their critical role of preparing for emergencies and protecting community health [17]. Given the global experience with the COVID-19 pandemic, it is relevant to explore how the evidence base has developed since the framework and indicators were created, with a focus on infectious disease preparedness.
In this scoping review, we explored the literature on frameworks, priority areas and indicators for PHEP with a focus on infectious disease emergencies. We used the Resilience Framework for PHEP to examine areas of preparedness actions and indicators developed in the period since the previous scoping review was conducted in 2017 [19], which includes the COVID-19 pandemic period. The objective of this scoping review is to investigate the following two research questions:
-
1.
What recent evidence has emerged on conceptual frameworks for PHEP specific to pandemics and infectious disease emergencies?
-
2.
What recent evidence has emerged pertaining to measurement of preparedness for pandemics and infectious disease emergencies?
Methods
Aim and design
A scoping review methodology was used, given the exploratory nature of the research questions. The Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist reporting on this scoping review is provided in additional file 3 [20]. Scoping reviews focus on mapping concepts underpinning a research area and are useful when examining areas that are emerging, to clarify key concepts and identify gaps [20,21,22,23,24]. Levac et al. (2010), describe how scoping review methodology allows for iterative processes and refinements while conducting a review [23]. In addition, Peters et al. (2020), describe how a variety of evidence and information sources may be used in scoping reviews, informing the objectives and approach for this scoping review [24]. The aim of this review was to expand understandings of the current state of PHEP frameworks, priority areas and indicators relevant to public health agencies, and how the evidence may have evolved during the COVID-19 pandemic. As has been described for scoping review methodology, a quality appraisal of the included studies was not conducted for this exploratory review [21,22,23]. The focus of this review was on local and/or regional or provincial/state (i.e. sub-national) public health, given that the public health system in Canada is organized around local/regional public health agencies, with provincial health system governance and organization [18, 19].
Data sources and search methods
Library information specialists at Public Health Ontario (PHO) were consulted to conduct database searches in MEDLINE (March 22, 2022); Embase, Business Continuity & Disaster Recovery Reference Center and Scopus (March 28, 2022); and the National Institutes of Health COVID-19 Portfolio for Preprints (March 15, 2022). The search included terms related to public health emergencies, emergency preparedness, post-pandemic recovery, indicators/measures, and frameworks.
The indexed literature search focused on identifying publications that included a description of frameworks, tools, models, activities or indicators for emergency preparedness for infectious diseases, pandemic influenza and the COVID-19 pandemic from 2017 onward. This approach captured literature published since the scoping review was conducted to inform the Delphi expert panel for PHEP indicator development [19], as well as literature published during the COVID-19 pandemic.
In addition to the indexed literature, a grey literature search was conducted from March 17, 2022 to March 25, 2022. PHO library information specialists were consulted to develop search strings to be used in Google Custom Search Engines and select regional, national and international public health agency websites. The search was limited to records published from 2020 onward to capture frameworks, models, toolkits and indicators published within the COVID-19 pandemic context. See additional file 1 for the full indexed and grey literature search strategies.
Eligibility criteria and record selection
The eligibility criteria were the same across indexed and grey literature except for the time periods searched, as noted above. Records were included in the scoping review if they met the following criteria: (a) planning, readiness and preparedness included the roles and responsibilities of local, regional or provincial/state/sub-national public health agencies relevant to Canada; (b) emergency described in the article or framework was a pandemic and/or of infectious origins; (c) the emergency or framework described was specific to an Organization for Economic Co-operation and Development (OECD) country; and (d) described preparedness activities, including indicators to inform preparedness activities, that are under local, regional or provincial/state (i.e. sub-national) level jurisdiction. We included relevant evidence from reviews, grey literature reports and primary research studies of any study design [24].
Records describing federal-, national-, or international-level (e.g., WHO) relevant frameworks or indicators were also included if the roles, responsibilities, elements and/or indicators described were relevant to public health agencies and public health system organization in Canada. For example, frameworks that described surveillance and laboratory testing activities were included, whereas a focus on measures relevant only to the federal level in Canada such as travel quarantine would be excluded. Infectious disease emergency was defined as an incident, outbreak or threat with the potential to overwhelm or otherwise disrupt routine local capacities due to their timing, scale or unpredictability [16, 25, 26]. Only English-language records were included.
Records were excluded if they: (a) focused on non-preparedness components of emergency management (i.e., response, recovery and mitigation); (b) described an emergency of non-infectious origins; (c) described a framework limited to country or federal-level roles relevant to Canada and countries with similar health system organization; or (d) focused on health care system (e.g., primary care, acute care) preparedness without public health system considerations [18]. Commentaries were excluded.
Results of the indexed literature search were pilot-screened by two authors. A random selection of 100 records were first screened independently in duplicate to check agreement and trial the eligibility criteria, which achieved 84% agreement. This allowed the two authors to discuss discrepancies and reach consensus on the articles, leading to enhanced understanding and consistency in how the remaining records were screened. Single author screening occurred for the remainder of indexed literature results, and a third author was consulted for uncertainties related to inclusion of specific studies when required. The grey literature search and screening were conducted by two authors. Similar to the process for indexed literature, a third author was consulted for uncertainties related to the inclusion of grey literature records when required.
Data extraction, summary and synthesis
The following details were extracted from the included publications: year, country/jurisdiction, relevant jurisdictional level (e.g., national, provincial, regional, or local/municipal), type of infectious disease emergency (i.e., COVID-19, any infectious disease), study and/or framework design and objective(s), description of the framework’s elements or components, and description of the framework indicators (if applicable). For records related to all-hazards PHEP, only details relevant to infectious diseases were extracted. While single-author extraction was conducted for the indexed and grey literature, frequent consultation amongst reviewers occurred throughout this process to support agreement.
The first step in analysis was identifying elements and emergent themes from the included publications. Given that the previous research by Khan et al. identified 11 essential elements of PHEP relevant to the Canadian context, and this review was conducted in Ontario, Canada, the elements of the Resilience Framework for PHEP were used as a reference point to organize the findings deductively (see additional file 2 for the detailed description of elements) [17, 19]. At the time of this scoping review, Khan et al.’s publication was the only rigorously developed PHEP framework specific to the Canadian context known to this research team [17,18,19]. The previous research used the term “elements” to refer to high-level topic areas related to public health preparedness, which are associated with indicators [18, 19]. In this review, we use the term elements when referring to the Resilience Framework for PHEP directly, and to reflect when new content aligned with the elements as they are described in the Resilience Framework for PHEP. Although Khan et al.’s work examined preparedness for all-hazards emergencies, the scope of this review was focused on identifying emerging themes related to public health preparedness for infectious disease emergencies, including pandemics. For the purposes of identifying gaps or new areas of preparedness, we refer to the high-level topic areas related to public health preparedness for infectious disease emergencies identified in publications as “emergent themes”. Publications included in this review used various terms including “principles”, “domains”, “elements”, “dimensions”, “key areas”, “categories” and others which could be associated with related actions or indicators in a similar approach to the Resilience Framework for PHEP. Our research team selected one term, “emergent themes”, to encompass these varied terms. Ethics and values were considered as part of the 11 elements, rather than separate, consistent with the Resilience Framework for PHEP [17].
In the second step, emergent themes were compared and contrasted with the elements of the Resilience Framework for PHEP to examine similarities and/or differences [17]. We identified elements of the Resilience Framework for PHEP that were described in the literature, and preparedness themes that emerged since the previous scoping review and indicator development work of Khan, et al. [18, 19], and since the COVID-19 pandemic. Where alignment was observed, we report how frequently each element was observed across included publications. When themes did not explicitly overlap with the Resilience Framework for PHEP, as determined by discussion and consensus among authors, these were recorded as “emergent themes”. The indexed and grey literature were analyzed separately and then synthesized across all results. Team members compared their lists of emergent themes, and where appropriate, aligned the language to consolidate and describe common emergent themes. We also included select examples of preparedness activities relevant to various PHEP elements and emergent themes.
The final step was to examine included studies for indicators or actions/activities that could be used to inform the development of indicators. Indicators were defined as succinct measures that help understand, compare and improve systems [27]; they are generally found in frameworks, assessment tools or checklists. The identification and appropriate synthesis of specific PHEP indicators was not feasible for this review. For subsequent indicator development, additional steps in indicator development are required to extract and analyze indicators identified in the literature. For the purposes of this review, broad areas of measurement (e.g., population vaccination coverage) were synthesized rather than specific indicators (e.g., specific quantitative thresholds for vaccine coverage) from a given framework or publication.
Results
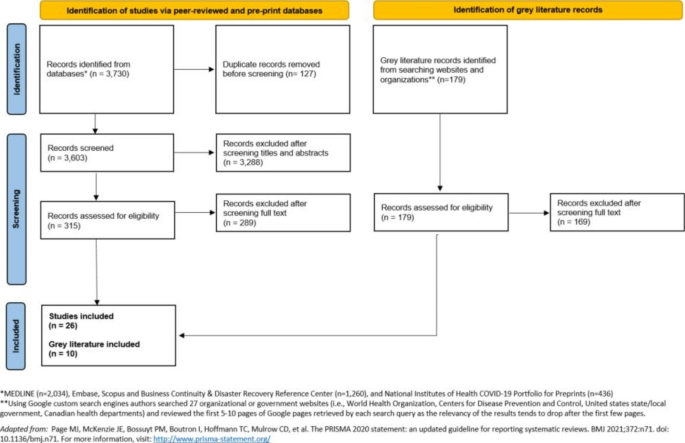
From the 3,603 records identified through the peer-reviewed and pre-print literature database searches, 315 full-text records were assessed for eligibility and 26 studies were included in this scoping review. Of the records identified from searching organizational or government databases in the grey literature search, 179 were assessed for eligibility and 10 grey literature publications were included in this scoping review (see PRISMA diagram in Fig. 1). In summary, 36 records were examined for this scoping review.
Characteristics of included publications
Methods and study designs varied widely across the 26 indexed literature studies, including systematic literature reviews [28,29,30], mixed-methods studies (i.e., a paper that describes a literature review, concept mapping and key informant interviews) [31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46], descriptive case studies [47,48,49], qualitative studies [50, 51], a cross-sectional study [52], and a regression analysis [53]. Ten studies described a PHEP-related framework, tool or model [33,34,35,36,37, 39,40,41,42, 44], and 16 studies included content relevant to PHEP priority areas and/or activities but did not explicitly describe a PHEP framework, tool, model or set of indicators [28,29,30,31,32, 38, 43, 45,46,47,48,49,50,51,52,53]. For example, two studies specifically focused on the community engagement component of PHEP [51, 52]. All studies identified from the indexed literature described PHEP concepts for infectious disease outbreaks, pandemic influenza and/or the COVID-19 pandemic.
A total of 10 grey literature publications were identified, including four that described PHEP frameworks or conceptual models [54,55,56,57], three that described assessment tools [58,59,60], and three that focused on indicators for PHEP [61,62,63]. All ten grey literature publications described public health preparedness actions for infectious disease outbreaks, COVID-19 pandemic or zoonotic disease outbreaks. Of the ten documents identified, seven were produced by the WHO [54,55,56,57,58,59,60]. Upon identification and review of the heterogeneous evidence and guidance, we oriented this scoping review around distilling findings into high-level concepts and themes relevant to PHEP.
Elements from the Resilience Framework for PHEP that appeared in the included publications
After the first and second steps in analysis of the included studies, at least one element from the Resilience Framework for PHEP was observed in all of the identified 26 indexed studies [28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53], and seven of the ten grey literature records [54,55,56,57,58,59,60], with many publications making reference to multiple elements (see Table 1). The 11 elements, listed from most to least frequently observed across the included publications, were: collaborative networks, community engagement, risk analysis, communication, planning process, governance and leadership, surveillance and monitoring, resources, workforce capacity, learning and evaluation, and practice and experience.
Emerging preparedness themes that expand on the elements in the Resilience Framework for PHEP
After comparing and contrasting as part of analysis, our synthesis resulted in the identification of ten themes that expand on the elements in the Resilience Framework for PHEP [17], all with a focus on infectious disease emergency preparedness (see Table 2). Five themes that expand on the framework were observed across both the indexed and grey literature; ordered from most to least common according to the number of publications in which they appear, these themes were: planning to mitigate inequities, building vaccination capacity, research and evidence-informed decision making, building laboratory and diagnostic system capacity, and building infection prevention and control (IPAC) capacity. There were three themes that expand on the Resilience Framework for PHEP that emerged solely from the indexed literature (climate and environmental health, public health legislation, phases of preparedness) and two that emerged solely from the grey literature (financial investment in infrastructure, and health system capacity).
Most publications described activities that should take place while planning or preparing for infectious disease emergencies to operationalize priority areas of preparedness [28,29,30,31,32, 35, 36, 38, 39, 41,42,43, 45,46,47,48,49, 51, 52, 54, 55, 58, 60]. Activities correspond with various preparedness priority areas and exemplify actions that would be taken during infectious disease emergency preparedness processes. These activities were described in publications in addition to or in place of indicators. Activities were described in a variety of ways across publications, and included steps, actions, suggestions, outcomes or outputs of infectious emergency preparedness planning processes.
Multiple studies from the indexed literature described activities related to the operationalization of preparedness [28,29,30,31,32, 35, 36, 38, 39, 41,42,43, 45,46,47,48,49, 51, 52]. For example, Jesus et al. (2021)’s model for disability-inclusiveness in pandemic preparedness provided several preparedness activities, some of which included developing intersectoral disability-inclusive pandemic preparedness, using evidence on how to reduce disability disparities to inform planning, and the reinforcement of disability-rights in health professionals’ education [36]. AuYoung et al. (2022) developed general strategies for COVID-19 vaccine hesitancy among marginalized communities relevant to future public health emergencies [47]. Examples of AuYoung et al.’s strategies include increasing community and academic capacity to enhance community-academic partnerships, investing in trusted messengers, increasing the trustworthiness of academic institutions and developing long-term cross-site partnerships [47]. Tan et al. (2021) investigated qualitative factors related to pandemic preparedness and identified strategies to achieve a more holistic and equitable approach to preparedness [43]. According to Tan et al., the ongoing translation of changing scientific evidence into policy actions and the development of trusted communication through effective knowledge translation practices are essential strategies to achieve evidence-informed decision-making in pandemic preparedness [43]. Tan et al. also put forward suggestions related to ecological determinants of health which overlap with disaster risk reduction strategies [64, 65], including addressing the effect of health services on the environment, recognizing the impact of climate and environmental degradation on risk of zoonotic disease, and setting climate goals [43].
Several preparedness frameworks identified in the grey literature included preparedness activities, outputs or outcomes [54, 55, 58, 60]. The WHO’s Strategic Preparedness, Readiness and Response Plan to End the Global COVID-19 Emergency in 2022 describes approaches to managing misinformation, such as peer-to-peer interventions to help communities identify accurate vaccine information by building resilience against misinformation [54]. The WHO’s Strategic Toolkit for Assessing Risks for All-hazards Emergencies lists expected activities and outputs of applying the toolkit’s six steps, one such activity is a gap analysis that can inform health and public health workforce capacity building [58]. The WHO’s Risk Communication and Community Engagement tool included a list of open-ended questions intended for use within focus group discussions or key informant interviews to support preparedness planning for risk communication and community engagement [60]. Together, these activities and outputs help to operationalize priority areas of infectious disease preparedness.
Preparedness indicators
In the final step of analysis we examined studies for available indicators or actions/activities to inform indicator development. Compared to the literature identified on frameworks and priority areas for preparedness, there were comparatively fewer indexed and grey literature records identified that describe qualitative and quantitative preparedness indicators. Five indexed studies [33, 34, 37, 40, 44] and three grey literature documents [61,62,63] either included or focused on describing indicators for pandemic and infectious disease preparedness. As described in the methods, we aimed to summarize areas of preparedness measurement, rather than specific quantitative thresholds or indicators. Our focus on areas of measurement rather than specific indicators allow public health agencies to tailor these areas of measurement to their preparedness context (e.g., local, regional or provincial).
The types of infectious disease preparedness indicators identified in this scoping review measured or assessed various areas of preparedness including the equity impacts of emergencies [34, 44, 62], core public health and government capacities for emergency preparedness and response [33, 63], population and healthcare system vulnerabilities during pandemics [40], community readiness [37], and benchmarks to strengthen health systems during outbreaks [61]. Some examples of indicators related to public health and health system readiness or capacity include: adequate public health budget [62, 63], capacity to deliver vaccines and the proportion of the population getting vaccinated [33, 61, 63], licensed nurses’ ability to practice in other regions or states [63], oversight of research on dangerous pathogens [61], and enhanced training for the safe transportation of biohazards [61].
Some examples of equity-related preparedness indicators identified through this review are: proportion of population in a defined region who are racialized or first-generation immigrants [34], benchmarks for public health agency plans to embed the needs of racialized or marginalized populations [62], proportion of population with access to internet and technology [44], ratio of residential and nursing homes per 10,000 population aged over 70 years old [40], proportion of population with access to clean water [63], and the proportion of households with at least one of the following: no kitchen, no plumbing, high cost of living, or overcrowded living conditions [37].
Discussion
This scoping review examined the recent literature on conceptualizing, defining and measuring PHEP, which is of relevance to public health agencies as they continue to respond to the COVID-19 pandemic, and remain ready for future infectious disease emergencies. Recent literature on infectious disease emergencies was compared with an evidence-based Resilience Framework for PHEP, which encompasses both infectious and non-infectious emergencies [17, 18]. Collaborative networks, community engagement, risk analysis and communication were the Resilience Framework elements most frequently observed across the publications included in this review. For example, collaborative networks was defined as the development of relationships, partnerships and strong networks in the Resilience Framework for PHEP (see additional file 2) [17]. In this review, 22 of 36 publications demonstrated this element, such as a WHO Framework which listed multisectoral coordination as one of its eight key areas for preparedness, calling for coordination across sectors and partners to ensure coherence in preparedness activities and increase resilience [56]. Community engagement was defined in the Resilience Framework in terms of understanding and engaging with the community; we identified 21 publications that demonstrated this element. For example, two publications specifically examined activities that facilitated or improved community engagement in emergency preparedness at the local health department level [51, 52]. In general, there was alignment between the themes that emerged from the studies identified and the elements in the Resilience Framework for PHEP.
Several themes identified in this review expand on the Resilience Framework for PHEP specifically in the context of pandemic and infectious disease preparedness. These emergent themes highlight the importance of planning to mitigate inequities, increasing scientific capacity (research and evidence-informed decision making) and increasing public health capacity (building vaccination capacity, building laboratory capacity, building IPAC capacity). These emergent themes represent areas of PHEP that warrant enhanced consideration for infectious disease emergencies. Other operational frameworks and relevant corresponding indicators could be used to augment areas for action specific to infectious diseases; for example, the WHO published an updated Joint External Evaluation (JEE) tool in June 2022, after the search date of this review [66]. It will be important to examine the tools, approaches and new knowledge that emerge as recovery from the COVID-19 pandemic evolves.
Planning to mitigate inequities emerged as an important theme across many included publications. Population health inequities were present and known prior to the COVID-19 pandemic; however, the pandemic re-focused attention on the need for equity-oriented actions due to the inequitable burden of COVID-19 morbidity and mortality, and disproportionate impact of both implementation and removal of pandemic-related response measures among marginalized communities [7,8,9]. Several publications highlighted the importance of anticipating and mitigating inequitable impacts resulting from infectious disease emergencies and related emergency response measures on marginalized populations [28, 29, 34, 36,37,38,39,40,41,42,43,44,45,46,47,48, 52, 54, 56]. Studies described a variety of equity considerations for preparedness, including the importance of monitoring baseline population characteristics, fostering community trust, and planning for material or financial supports for those inequitably impacted. In addition, infectious disease preparedness frameworks identified in the grey literature provided examples of preparedness activities that help to mitigate inequities related to infectious public health emergencies, including the engagement of trusted community members to ensure communications reach marginalized populations [67]. The Resilience Framework for PHEP includes ethics and values as a concept that is core to all elements in the framework to ensure PHEP actions are ethics-informed. The emergent theme of mitigating inequities in this scoping review reinforces that equity, as an ethical value important in public health, should also be explicitly incorporated as a foundational component of future preparedness frameworks, efforts and actions.
Research and evidence-informed decision-making are central concepts in public health practice and important for emergency preparedness. This theme was often discussed in the indexed literature and was the most frequently observed theme in the grey literature [30, 32, 42, 43, 54, 56,57,58]. These publications discussed the importance of knowledge-sharing networks, building capacities for data collection, analysis, and research generation to ensure that infectious disease preparedness activities are evidence-informed. This emergent theme is an example of how themes identified through this scoping review intersect and overlap with other emergent themes as well as elements of the Resilience Framework for PHEP [17, 18]. For example, building capacity for research and evidence-informed decision-making across governments, communities and non-governmental agencies requires action related to mitigating inequities, communication, community engagement, collaborative networks, surveillance and monitoring, among others.
Building vaccination and laboratory capacity, climate health, and public health legislation are additional preparedness considerations that reflect changes to PHEP planning that were in progress before the pandemic and have received renewed attention during the COVID-19 pandemic. Public confidence in vaccination is an example of the need for management of public health misinformation that pre-dates, and was further exacerbated by, the COVID-19 pandemic. Several publications discussed vaccination and laboratory systems as key components of the COVID-19 response as well as important priority areas for future pandemic planning [30, 43, 47,48,49, 53, 54]. Considerations for climate and environmental health and public health legislation are broad topics that have garnered renewed attention for preparedness in light of the COVID-19 pandemic. Publications that included climate or environmental considerations noted the complex relationship between these issues and potential future pandemics due to climate change and environmental degradation increasing the risk of zoonotic diseases crossing over to humans, and the contributions of healthcare and pandemic response operations to waste, emissions and potential environmental contamination [41,42,43]. While governance and leadership is a cross-cutting element in the Resilience Framework for PHEP, the COVID-19 pandemic has renewed an interest in clearly articulating public health emergency roles and responsibilities in public health legislation; thus, providing legislative or policy support for public health emergency decision-making [68].
Themes that expand on the Resilience Framework for PHEP [17, 18] represent potential areas for improvement in the public health and the health system in general, and are not all specific to infectious disease and pandemic preparedness. For example, the domains of financial investment in infrastructure, and health system capacity are areas of focus with population-level health benefits that extend beyond preparedness for public health emergencies and infectious diseases. Several publications highlighted the need for investments to build strong and resilient health and public systems to mitigate the impacts of a health emergency and reduce disruption to essential health and public health services. The COVID-19 pandemic may have exposed these areas of weakness; however, these aspects of the public health system required attention and improvement prior to and beyond the pandemic as noted in previous reports on the impact of the SARS-CoV-1 pandemic [69, 70]. While pandemic and emergency-specific surge capacities and plans are needed, an adequate and resilient baseline is also required.
This scoping review identified emerging priority areas for action in infectious disease emergency preparedness; however, there were comparatively fewer records identified that describe qualitative and quantitative preparedness indicators published since evidence-based indicator development by Khan et al. [19]. Detailed analysis, evaluation and indicator development was beyond the scope of this review, although the findings suggest areas of focus that should be considered in future planning. Of note, an exploratory analysis of pandemic preparedness compared with pandemic outcomes posited that some existing preparedness indices are not well suited to predicting pandemic outcomes, but instead are better served as tools to highlight gaps in pandemic capacities [71]. Further work is needed in development of indicators, and also their validation in relation to relevant outcomes. In addition, continued work is needed to ensure preparedness is reinforced as a dynamic, adaptive concept, consistent with complex adaptive systems theory. Anchoring preparedness, planning, and readiness as upstream activities to support resilience of the system can support the concept of the work as continuous improvement and adaptation [18]. The COVID-19 pandemic continues to evolve globally, and jurisdictions are still engaged in the pandemic response and may not yet have capacity to explore how the pandemic might change their approach to emergency planning moving forward. In the coming months and years, there will likely be additional evidence to shape future preparedness planning that will include elements and/or indicators that will support effective infectious disease emergency preparedness. This future work should be revisited, examined and documented to ensure that learning from the pandemic response is included in future preparedness planning domains, activities and indicators.
Limitations
A limitation of this scoping review, common to review methodology, is that some relevant records may not have been included. Further, any ongoing work in jurisdictions and academia to update preparedness plans may not be publicly available since the pandemic response is ongoing, or may not be available in English. Although the search strategy employed was detailed and developed by library information specialists, key terms not included in the search may have led to some documents being excluded. Relevant work published after March 25, 2022, when our search was completed, would not be included. Due to the nature of the review, a risk of bias analysis was not conducted. Other methodological limitations, due to feasibility and time constraints, included: lack of a written protocol, single author screening, and single author extraction with a second author check. Mitigation strategies included a trial of eligibility criteria, frequent collaborative discussions and peer-review of work.
Future directions
Future work can advance knowledge related to the emergent themes identified and translate these findings into evidence-informed indicators for public health emergency preparedness. Strategies and indicators for mitigating inequities should be considered an urgent focus for action to support the reduction of health inequities anticipated for future emergencies. Future work is also required to extract and analyze indicators for PHEP identified in the recent literature, as well as validate existing indicators in practice.
Conclusion
The 11 elements of an evidence-based pre-COVID-19 pandemic, all-hazards Resilience Framework for PHEP developed in Canada relevant to local or regional public health agencies continue to be reflected in the literature identified in this scoping review. In the studies identified in this review, the following elements in the Resilience Framework for PHEP were represented in descending order of frequency: collaborative networks, community engagement, risk analysis, communication, planning process, governance and leadership, surveillance and monitoring, resources, workforce capacity, learning and evaluation, and practice and experience. This scoping review focused on infectious disease emergencies and through our analysis identified additional areas of preparedness actions that pertain to the emergent themes of mitigating inequities, public health capacities, scientific capacities, and considerations for health system capacity. Planning to mitigate inequities was a particularly important and frequently observed theme across the included publications, and one that warrants additional attention and efforts to operationalize into PHEP practice.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
- COVID-19:
-
Coronavirus Disease 2019
- IPAC:
-
Infection Prevention and Control
- JEE:
-
Joint External Evaluation
- OECD:
-
Organization for Economic Co-operation and Development
- PHEP:
-
Public health emergency preparedness
- PHO:
-
Public Health Ontario
- SARS:
-
Severe acute respiratory syndrome
- WHO:
-
World Health Organization
References
Stoddard M, Sarkar S, Yuan L, Nolan RP, White DE, White LF, et al. Beyond the new normal: assessing the feasibility of vaccine-based suppression of SARS-CoV-2. PLoS ONE. 2021;16(7):e0254734.
Our World in Data. Cumulative confirmed COVID-19 deaths. Global Change Data Lab, Oxford. 2022. https://ourworldindata.org/explorers/coronavirus-data-explorer?zoomToSelection=true&time=2020-03-01.latest&facet=none&pickerSort=desc&pickerMetric=total_cases&hideControls=true&Metric=Confirmed+deaths&Interval=Cumulative&Relative+to+Population=false&Color+by+test+positivity=false&country=~OWID_WRL. Accessed 11 Oct 2022.
Fussell E, Sastry N, Vanlandingham M. Race, socioeconomic status, and return migration to New Orleans after Hurricane Katrina. Popul Environ. 2010;31(1–3):20–42.
Tricco ACLE, Soobiah C, Perrier L, Straus SE. Impact of H1N1 on socially disadvantaged populations: systematic review. PLoS ONE. 2012;7(6):e39437.
Wellesley Institute. Tracking COVID-19 through race-based data. Wellesley Institute, Toronto. 2021. https://www.wellesleyinstitute.com/wp-content/uploads/2021/08/Tracking-COVID-19-Through-Race-Based-Data_eng.pdf. Accessed 16 May 2022.
Khanijahani A, Iezadi S, Gholipour K, Azami-Aghdash S, Naghibi D. A systematic review of racial/ethnic and socioeconomic disparities in COVID-19. Int J Equity Health. 2021;20(1):248.
; Public Health Agency of Canada, Tam T. From risk to resilience: an equity approach to COVID-19. Public Health Agency of Canada, Ottawa. 2020. https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/from-risk-resilience-equity-approach-covid-19.html. Accessed 15 Aug 2022.
Ismail SJ, Tunis MC, Zhao L, Quach C. Navigating inequities: a roadmap out of the pandemic. BMJ Global Health. 2021;6(1):e004087.
McGrail K, Morgan J, Siddiqi A. Looking back and moving forward: addressing health inequities after COVID-19. Lancet Reg Health Am. 2022;9:100232.
Sabin NS, Calliope AS, Simpson SV, Arima H, Ito H, Nishimura T, et al. Implications of human activities for (re)emerging infectious diseases, including COVID-19. J Physiol Anthropol. 2020;39(1):29.
Venkatesan P. Re-emergence of infectious diseases associated with the past. Lancet Microbe. 2021;2(4):e140.
McCloskey B, Dar O, Zumla A, Heymann DL. Emerging infectious diseases and pandemic potential: status quo and reducing risk of global spread. Lancet Infect Dis. 2014;14(10):1001–10.
World Health Organization. A strategic framework for emergency preparedness. World Health Organization, Geneva. 2017. https://extranet.who.int/sph/sites/default/files/document-library/document/Preparedness-9789241511827-eng.pdf. Accessed 27 Apr 2022.
Khan Y, Fazli G, Henry B, de Villa E, Tsamis C, Grant M, et al. The evidence base of primary research in public health emergency preparedness: a scoping review and stakeholder consultation. BMC Public Health. 2015;15:432.
Lee AC, Phillips W, Challen K, Goodacre S. Emergency management in health: key issues and challenges in the UK. BMC Public Health. 2012;12:884.
Nelson C, Lurie N, Wasserman J, Zakowski S. Conceptualizing and defining public health emergency preparedness. Am J Public Health. 2007;97(Suppl 1):9–11.
Ontario Agency for Health Protection and Promotion (Public Health Ontario). Public health emergency preparedness framework and indicators: a workbook to support public health practice. King’s Printer for Ontario, Toronto. 2020. https://www.publichealthontario.ca/-/media/Documents/W/2020/workbook-emergency-preparedness.pdf?sc_lang=en. Accessed 27 Apr 2022.
Khan Y, O’Sullivan T, Brown A, Tracey S, Gibson J, Généreux M, et al. Public health emergency preparedness: a framework to promote resilience. BMC Public Health. 2018;18(1):1344.
Khan Y, Brown AD, Gagliardi AR, O’Sullivan T, Lacarte S, Henry B, et al. Are we prepared? The development of performance indicators for public health emergency preparedness using a modified Delphi approach. PLoS ONE. 2019;14(12):e0226489.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015 Sep;13(3):141–6.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69.
Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Chapter 11: scoping reviews (2020 version). In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI, 2020. https://doi.org/10.46658/JBIMES-20-12. Accessed 9 Jan 2023.
Khan Y, Sanford S, Sider D, Moore K, Garber G, de Villa E, et al. Effective communication of public health guidance to emergency department clinicians in the setting of emerging incidents: a qualitative study and framework. BMC Health Serv Res. 2017;17(1):312.
Paek HJ, Hilyard K, Freimuth V, Barge JK, Mindlin M. Theory-based approaches to understanding public emergency preparedness: implications for effective health and risk communication. J Health Commun. 2010;15(4):428–44.
United Kingdom. National Health Service Institute for Innovation and Improvement. The good indicators guide: understanding how to use and choose indicators. National Health Service, London. 2017. https://www.england.nhs.uk/improvement-hub/wp-content/uploads/sites/44/2017/11/The-Good-Indicators-Guide.pdf. Accessed 27 Apr 2022.
Savoia E, Lin L, Bernard D, Klein N, James LP, Guicciardi S. Public health system research in public health emergency preparedness in the United States (2009–2015): actionable knowledge base. Am J Public Health. 2017;107(S2):e1–e6.
Williams BE, Kondo KK. Preventing unequal health outcomes in COVID-19: a systematic review of past interventions. 2021;5(1):856–71.
Yoon YK, Lee J, Kim SI, Peck KR. A systematic narrative review of comprehensive preparedness strategies of healthcare resources for a large resurgence of COVID-19 nationally, with local or regional epidemics: present era and beyond.J Korean Med Sci. 2020;35(44).
Aruru M, Truong HA, Clark S. Pharmacy emergency preparedness and response (PEPR): a proposed framework for expanding pharmacy professionals’ roles and contributions to emergency preparedness and response during the COVID-19 pandemic and beyond. Res Social Adm Pharm. 2021;17(1):1967–77.
Bardosh KL, de Vries DH, Abramowitz S, Thorlie A, Cremers L, Kinsman J, et al. Integrating the social sciences in epidemic preparedness and response: a strategic framework to strengthen capacities and improve global health security. Global Health. 2020;16(1):120.
Boyce MR, Katz R. Rapid urban health security assessment tool: a new resource for evaluating local-level public health preparedness. BMJ Glob Health. 2020;5(6):e002606.
Brakefield WS, Ammar N, Olusanya OA, Shaban-Nejad A. An urban population health observatory system to support COVID-19 pandemic preparedness, response, and management: design and development study. JMIR Public Health Surveill. 2021;7(6):e28269.
de Rooij D, Belfroid E, Eilers R, Roßkamp D, Swaan C, Timen A. Qualitative research: institutional preparedness during threats of infectious disease outbreaks. Biomed Res Int. 2020. https://doi.org/10.1155/2020/5861894.
Jesus TS, Kamalakannan S, Bhattacharjya S, Bogdanova Y, Arango-Lasprilla JC, Bentley J, et al. PREparedness, REsponse and SySTemic transformation (PRE-RE-SyST): a model for disability-inclusive pandemic responses and systemic disparities reduction derived from a scoping review and thematic analysis. Int J Equity Health. 2021;20(1):204.
Links JM, Schwartz BS, Lin S, Kanarek N, Mitrani-Reiser J, Sell TK, et al. COPEWELL: a conceptual framework and system dynamics model for predicting community functioning and resilience after disasters. Disaster Med Public Health Prep. 2018;12(1):127–37.
Maqbool A, Khan NZ. Analyzing barriers for implementation of public health and social measures to prevent the transmission of COVID-19 disease using DEMATEL method. Diabetes Metab Syndr. 2020;14(5):887–92.
Meyer D, Bishai D, Ravi SJ, Rashid H, Mahmood SS, Toner E, et al. A checklist to improve health system resilience to infectious disease outbreaks and natural hazards. BMJ Glob Health. 2020;5(8):e002429.
Nicodemo C, Barzin S, Cavalli N, Lasserson D, Moscone F, Redding S, et al. Measuring geographical disparities in England at the time of COVID-19: results using a composite indicator of population vulnerability. BMJ Open. 2020;10(9):e039749.
Sell TK, Shearer MP, Meyer D, Chandler H, Schoch-Spana M, Thomas E, et al. Public health resilience checklist for high-consequence infectious diseases-informed by the domestic ebola response in the United States. J Public Health Manag Pract. 2018;24(6):510–8.
Tagarev T, Ratchev V. A taxonomy of crisis management functions. Sustainability. 2020;12(12):5147.
Tan MMJ, Neill R, Haldane V, Jung A-S, De Foo C, Tan SM, et al. Assessing the role of qualitative factors in pandemic responses. BMJ. 2021;375:e067512.
Wong EY, Schachter A, Collins HN, Song L, Ta ML, Dawadi S, et al. Cross-sector monitoring and evaluation framework: social, economic, and health conditions impacted during the COVID-19 pandemic. Am J Public Health. 2021;111(S3):215–S23.
Choi H, Kim S-Y, Kim J-W, Park Y, Kim M-H. Mainstreaming of health equity in infectious disease control policy during the COVID-19 pandemic era. J Prev Med Public Health. 2021;54(1):1–7.
Glover RE, van Schalkwyk MCI, Akl EA, Kristjannson E, Lotfi T, Petkovic J, et al. A framework for identifying and mitigating the equity harms of COVID-19 policy interventions. J Clin Epidemiol. 2020;128:35–48.
AuYoung M, Rodriguez Espinosa P, Chen W-T, Juturu P, Young M-EDT, Casillas A et al. Addressing racial/ethnic inequities in vaccine hesitancy and uptake: lessons learned from the California alliance against COVID-19.J Behav Med. 2022.
Blouin Genest G, Burlone N, Champagne E, Eastin C, Ogaranko C. Translating COVID-19 emergency plans into policy: a comparative analysis of three canadian provinces. Policy Des Pract. 2021;4(1):115–32.
Schulze C, Welker A, Kühn A, Schwertz R, Otto B, Moraldo L et al. Public health leadership in a VUCA world environment: lessons learned during the regional emergency rollout of SARS-CoV-2 vaccinations in Heidelberg, Germany, during the COVID-19 pandemic.Vaccines. 2021;9(8).
Reddin K, Bang H, Miles L. Evaluating simulations as preparation for health crises like CoVID-19: insights on incorporating simulation exercises for effective response. Int J Disaster Risk Reduct. 2021;59:102245.
Schoch-Spana M, Ravi S, Meyer D, Biesiadecki L, Mwaungulu GJ. High-performing local health departments relate their experiences at community engagement in emergency preparedness. J Public Health Manag Pract. 2018;24(4):360–9.
Schoch-Spana M, Nuzzo J, Ravi S, Biesiadecki L, Mwaungulu G. Jr. The local health department mandate and capacity for community engagement in emergency preparedness: a national view over time. J Public Health Manag Pract. 2018;24(4):350–9.
Lee CT, Buissonnière M, McClelland A, Frieden TR. Association between preparedness and response measures and COVID-19 incidence and mortality. medRxiv. 2021. doi:https://doi.org/10.1101/2021.02.02.21251013.
World Health Organization. Strategic preparedness, readiness and response plan to end the global COVID-19 emergency in 2022. World Health Organzation, Geneva. 2022. https://www.who.int/publications/i/item/WHO-WHE-SPP-2022.1. Accessed 27 Apr 2022.
World Health Organization. Framework and toolkit for Infection prevention and control in outbreak preparedness, readiness and response at the national level. World Health Organization, Geneva. 2021. https://apps.who.int/iris/bitstream/handle/10665/345251/9789240032729-eng.pdf?sequence=1&isAllowed=y. Accessed 27 Apr 2022.
World Health Organization. Framework for strengthening health emergency preparedness in cities and urban settings. World Health Organization, Geneva. 2021. https://www.who.int/publications/i/item/9789240037830. Accessed 27 Apr 2022
World Health Organization. Pandemic influenza preparedness (PIP) framework for the sharing of influenza viruses and access to vaccines and other benefits, second edition. World Health Organization, Geneva. 2022. https://www.who.int/publications/i/item/9789240024854. Accessed 27 Apr 2022.
World Health Organization. Strategic toolkit for assessing risks: a comprehensive toolkit for all-hazards health emergency risk assessment. World Health Organization, Geneva. 2021. https://www.who.int/publications/i/item/9789240036086. Accessed 27 Apr 2022.
World Health Organization, Food and Agricultre Organization of the United Nations. Joint risk assessment operational tool (JRA OT): an operational tool of the tripartite zoonoses guide. World Health Organization, Geneva. 2020. https://apps.who.int/iris/bitstream/handle/10665/340005/9789240015142-eng.pdf?sequence=1&isAllowed=y. Accessed 27 Apr 2022
World Health Organization. Risk communication and community engagement action plan guidance: COVID-19 preparedness & response. World Health Organization, Geneva. 2020. https://www.who.int/publications/i/item/risk-communication-and-community-engagement-(rcce)-action-plan-guidance. Accessed 27 Apr 2022.
Bell JA, Nuzzo JB, Britsol N, Essix G, Isaac C, Kobokovich A et al. Global health security index 2021: advancing collective action and accountability amid global crisis. John’s Hopkins Center for Health Security, Baltimore. 2021. https://www.centerforhealthsecurity.org/our-work/publications/GHSindex2021. Accessed 18 July 2022.
National Collaborating Centre for Infectious Diseases. Measuring what counts in the midst of the COVID-19 pandemic: equity indicators for public health [Internet]. National Collaborating Centre for Infectious Diseases, Winnipeg. 2021. https://nccid.ca/publications/measuring-what-counts-in-the-midst-of-the-covid-19-pandemic-equity-indicators-for-public-health/. Accessed 18 Jul 2022.
Trust For America’s Health. Ready or not 2022: protecting the public’s health from diseases, disasters, and bioterrorism. Trust for America’s Health, Washington. 2022. https://www.tfah.org/report-details/ready-or-not-2022/. Accessed 18 July 2022.
United Nations Office for Disaster Risk Reduction. Sendai framework for disaster risk reduction 2015–2030. United Nations Office for Disaster Risk Reduction, Geneva. 2015. https://www.undrr.org/publication/sendai-framework-disaster-risk-reduction-2015-2030. Accessed 30 Sep 2022.
United Nations Framework Convention on Climate Change. Paris Agreement. United Nations Framework Convention on Climate Change, Geneva. 2015. https://unfccc.int/process-and-meetings/the-paris-agreement/the-paris-agreement#~:text=The%20Paris%20Agreement%20is%20a,compared%20to%20pre%2Dindustrial%20levels. Accessed 03 Sep 2022.
World Health Organization. Joint external evaluation tool: international health regulations (2005) - third edition. World Health Organization, Geneva. 2022. https://www.who.int/publications/i/item/9789240051980. Accessed 11 Jan 2023.
World Health Organization. Commission on social determinants of health final report. World Health Organization, Geneva. 2008. https://www.who.int/publications/i/item/9789241563703. Accessed 06 Sept 2022.
Network for Public Health Law and National Association of County and City Health Officials. Proposed limits on public health authority: dangerous for public health. Network for Public Health Law, Edina. 2021. https://www.naccho.org/uploads/downloadable-resources/Proposed-Limits-on-Public-Health-Authority-Dangerous-for-Public-Health-FINAL-5.24.21pm.pdf. Accessed 21 Sep 2022.
Health Canada. Learning from SARS: renewal of public health in Canada. Her Majesty the Queen in Right of Canada, Ottawa. 2003. https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/publicat/sars-sras/pdf/sars-e.pdf. Accessed 06 Sept 2022.
Campbell A. The SARS commission: SARS and public health in Ontario. Commission to Investigate the Introduction and Spread of SARS in Ontario, Toronto. 2006. http://www.archives.gov.on.ca/en/e_records/sars/report/index.html. Accessed 06 Sept 2022.
COVID-19 National Preparedness Collaborators. Pandemic preparedness and COVID-19: an exploratory analysis of infection and fatality rates, and contextual factors associated with preparedness in 177 countries, from Jan 1, 2020, to Sept 30, 2021. Lancet. 2022 Apr;16(10334):1489–512.
Acknowledgements
The authors gratefully acknowledge the support of Public Health Ontario’s Library Information Specialists, for their contributions to the indexed database and grey literature search strategies. The authors also acknowledge reviewers of earlier versions of this work, including Lori McKinnon of Public Health Ontario.
Funding
Not applicable. This study received no specific grant or funding.
Author information
Authors and Affiliations
Contributions
YK, JML, RJ, KES, FG, SKO and MM conceptualized the scoping review. JML, RJ, KES and FG identified, selected, extracted data in the included studies. JML, RJ, KES and FG wrote the manuscript of the scoping review with critical inputs and appraisal from YK and SKO. The manuscript was then reviewed by LEB, BS, MPL, MM and TLOS. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. Research ethics approval was not required for this scoping review as no humans or their tissues were involved.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lee, J.M., Jansen, R., Sanderson, K.E. et al. Public health emergency preparedness for infectious disease emergencies: a scoping review of recent evidence. BMC Public Health 23, 420 (2023). https://doi.org/10.1186/s12889-023-15313-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15313-7