- Research
- Open access
- Published:
The impact of ‘grounds’ on abortion-related outcomes: a synthesis of legal and health evidence
BMC Public Health volume 22, Article number: 936 (2022)
Abstract
Where abortion is legal, it is often regulated through a grounds-based approach. A grounds-based approach to abortion provision occurs when law and policy provide that lawful abortion may be provided only where a person who wishes to have an abortion satisfies stipulated ‘grounds’, sometimes described as ‘exceptions’ or ‘exceptional grounds’. Grounds-based approaches to abortion are, prima facie, restrictive as they limit access to abortion based on factors extraneous to the preferences of the pregnant person. International human rights law specifies that abortion must be available (and not ‘merely’ lawful) where the life or health of the pregnant woman or girl is at risk, or where carrying a pregnancy to term would cause her substantial pain or suffering, including but not limited to situations where the pregnancy is the result of rape or incest or the pregnancy is not viable. However, international human rights law does not specify a grounds-based approach as the way to give effect to this requirement. The aim of this review is to address knowledge gaps related to the health and non-health outcomes plausibly related to the effects of a grounds-based approach to abortion regulation. The evidence from this review shows that grounds have negative implications for access to quality abortion and for the human rights of pregnant people. Further, it shows that grounds-based approaches are insufficient to meet states’ human rights obligations. The evidence presented in this review thus suggests that enabling access to abortion on request would be more rights-enhancing than grounds-based approaches to abortion regulation.
Background
Where abortion is at least partially legal, it is commonly regulated through a grounds-based approach [1]. A grounds-based approach occurs when law and policy provides that lawful abortion may be availed of only where a person who wishes to have an abortion satisfies stipulated ‘grounds’, sometimes described as ‘exceptions’ or ‘exceptional grounds’. Grounds are defined as ‘circumstances under which abortion is lawful, that is, allowed or not contrary to law, or explicitly permitted or specified by law’ [2].
Typical ‘grounds’ include risk to the life or health of the pregnant woman, if the pregnancy results from rape, incest or sexual violence, severe or fatal fetal anomaly, or socio-economic grounds. However, grounds can be expressed in legal texts in ‘vague and confusing’ ways, making them even more difficult to implement [2]. In many cases these grounds-based approaches exist alongside and interact with other regulatory interventions such as gestational limits, third party authorization requirements, and criminalization to form a complex law and policy framework for abortion provision.
Grounds based approaches to abortion are, prima facie, restrictive as they limit access to abortion based on factors extraneous to the preferences of the pregnant woman. International human rights law (IHRL) specifies that abortion must be available (and not ‘merely’ lawful) where the life and health of the pregnant woman or girl is at risk, or where carrying a pregnancy to term would cause her substantial pain or suffering, including but not limited to situations where the pregnancy is the result of rape or incest or the pregnancy is not viable ([3], para 4). However, even though IHRL says abortion must be available in these circumstancs this does not mean that grounds-based approaches to abortion regulation are either mandated by or sufficient to satisfy IHRL. Rather, in ensuring that abortion is available in at least these circumstances states must be cognizant of, and must comply with, their broader IHRL obligations. These include obligations to take steps to ensure women do not have to undergo unsafe abortion ([4], para 6), to reduce maternal morbidity and mortality [3, 5], to effectively protect women and girls from the physical and mental risks associated with unsafe abortion [3, 5], to ensure that women’s and girls’ right to privacy and confidentiality in sexual and reproductive healthcare is protected, and to respect, protect and fulfil the broader right to the highest attainable standard of physical and mental health, including sexual and reproductive health.
The aim of this review is to address knowledge gaps related to the health and non-health outcomes that, while not directly linked through simple linear causal pathways, are plausibly related to the effects of a grounds-based approach to abortion regulation. The review followed a methodology for integrating human rights in guideline development that has been described elsewhere [6]. This methodology is well-suited to interventions that are complex, may have multiple interacting components, may be non-linear in their effects, and are often context dependent [7]. Such complex interventions often interact with one another, such that outcomes related to one individual or community may be dependent on others, and may be impacted positively or negatively by the people, institutions and resources that are arranged together within the larger system in which they are implemented [8]. This review was conducted as part of the evidence base for the World Health Organization (WHO)‘s recently-published Abortion Care Guideline [9]. It is one of seven reviews of evidence undertaken by the research team following the same methodological approach.
Throughout this review, and consistent with the approach in the Abortion Care Guideline ([9], p. xxii), we use the terms women, girls, pregnant women [and girls], pregnant people, and people interchangeably to include all those with the capacity to become pregnant.
Methods
Identification of studies and data extraction
This review examined the impact of the intervention of grounds-based approaches on two populations (i) people seeking abortion, and (ii) health professionals. Our study outcomes and search strategy were developed together with experts working in the fields of reproductive health, law, policy, and human rights. Our outcomes of interest included both health and non-health outcomes that, based on a preliminary assessment of the literature [10], could be linked to the effects of the ‘grounds’ intervention. Outcomes linked to those seeking abortion included delayed abortion, continuation of pregnancy, opportunity costs, reproductive coercion, and disproportionate impact. Outcomes linked to medical professionals included stigmatization, workload implications, referral of patients, and system costs.
We searched the databases PubMed, HeinOnline, and JStor and the search engine Google Scholar. The WHO’s Safe Abortion: technical and policy guidance for health systems (2nd edition) [11] included data up until 2012, thus, we limited our search to papers published in English after 2010 to the end of November 2020. We did not restrict on study design. We included only manuscripts that undertook original data collection or analysis i.e., quantitative studies (comparative and non-comparative), qualitative and mixed-methods studies, reports, PhD theses, and economic or legal analyses.
The full review team was comprised of four members (AC, FdL, MR and AL). FdL and AL developed the PICO question (People/Population/Patient; Intervention; Comparison (if applicable); Outcomes of Interest). Two reviewers (AC and FdL) conducted an initial screening of the literature. Titles and abstracts were first screened for eligibility using the Covidence® tool; full texts were then reviewed. A third reviewer (AL) confirmed that these studies met inclusion criteria. Two reviewers (FdL and AC) extracted data. Any discrepancies were reviewed and discussed with two additional reviewers (AL and MR). The review team resolved any discrepancies through consensus.
In order to fully understand the implications of the findings for abortion law and policy, we applied human rights standards to the data extracted from these manuscripts. The applicable standards were drawn from a review of the corpus of IHRL in accordance with the methodological approach applied [6]. They thus exclude regional and national human rights laws. The applicable standards were considered together with the evidence from the included manuscripts in order to identify, (a) which international human rights standards are engaged by grounds, (b) whether the evidence suggests that grounds have positive or negative effects on the enjoyment of rights, and (c) where no data are identified from the manuscripts against outcomes of interest, whether IHRL provides evidence that can further elucidate the impacts and effects of grounds. This is summarized in Tables 2 and 3 below.
Analysis
Data from included studies were matched to the outcomes and presented in Evidence tables. In these tables the impact of each finding on the outcome was presented, as well as an overall conclusion of the identified findings across outcomes of interest. To summarize the effect of the intervention, across all study designs, we utilized a previously developed approach and incorporated a visual representation of effect direction. The direction of the evidence was illustrated by a symbol which indicated whether, in relation to that particular outcome, the evidence extracted from a study suggested an increase (▲), decrease (⊽), or no change in the outcome (○). The symbol did not indicate the magnitude of the effect [6, 8].
Results
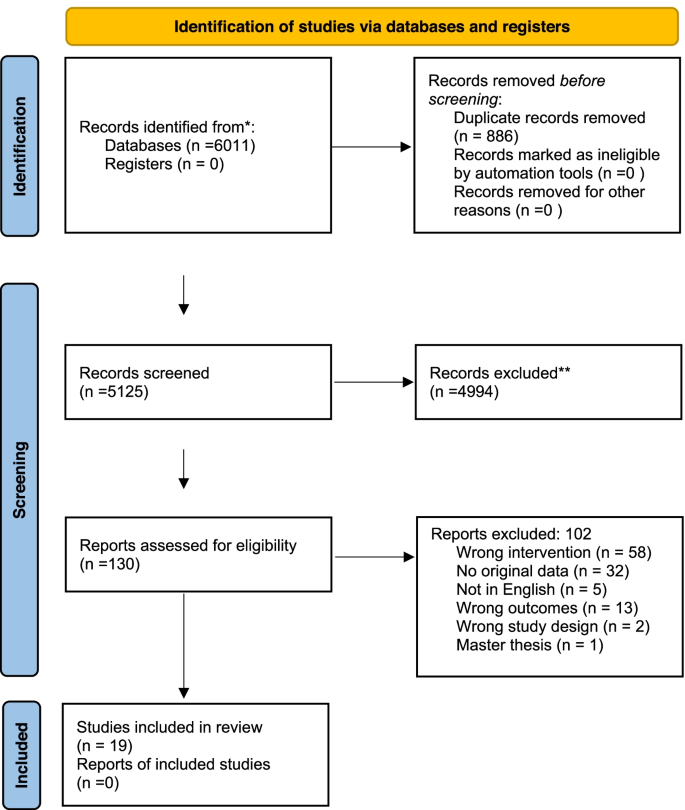
The initial search generated 5123 citations after duplicates were removed. We screened the titles and abstracts and conducted a full text screening of 130 manuscripts. After applying our exclusion criteria, 19 manuscripts were included in the final analysis (Fig. 1. Prisma flow diagram).
Prisma Flow diagram [12]
Manuscripts described data from the following settings: Argentina [13], Australia [14,15,16,17,18], Chile [19, 20], Colombia [21,22,23], Ethiopia [24], Ghana [25], Ireland [26, 27], Mexico [23, 28], Rwanda [29, 30], Thailand [31], United Kingdom/Great Britain [23, 32], and Uruguay [33]. The characteristics of included manuscripts are presented in Table 1. For the impact on people seeking abortion we included studies containing information relevant for the outcomes: delayed abortion [14, 20, 21, 27, 30] continuation of pregnancy [28, 33], opportunity costs [13,14,15,16, 20,21,22,23,24, 26, 29,30,31,32], self-managed abortion [26, 32], unlawful abortion [25, 26, 32], reproductive coercion [18, 24] and disproportionate impact [16, 18, 19, 23, 31]. For the impact on health professionals we included studies containing information relevant to workload implications [13, 18, 19, 24, 25], referral to another provider [14], imposition on conscience or ethics [19, 24], stigmatization [17], and system costs [18, 19, 27, 28, 33]. No evidence was identified linking the intervention to the outcomes: family disharmony, exposure to violence or exploitation, or impact on the provider-patient relationship.
Impact of grounds on abortion seekers
A summary of the impacts of grounds-based approaches on abortion seekers and the application to human rights are presented in Table 2. Evidence identified per study and outcome are presented in Supplementary Tables 1 and 2.
The evidence from six studies [14, 20, 21, 26, 27, 30] suggests that grounds-based approaches contribute to delays in accessing abortion. This includes delays resulting from inconsistencies in interpretation and application of grounds [21], questioning or ‘verification’ of women’s claims relating to grounds [14, 21], disagreement between medical professionals about whether a ground is satisfied [20], and health professionals delaying abortion until the pregnant person’s health condition is severe enough that the woman’s condition is deemed life threatening (and thus that a ‘risk to life’ ground is fulfilled) [20, 25]. The human rights standards reviewed make it clear that states must take steps to reduce maternal mortality and morbidity ([3, 5], paras [8, 10, 24, 30-33]), and to ensure that lawful abortion is safe and accessible [3]. The evidence from the reviewed studies suggests that grounds are associated with delay in a way that indicates incompatibility with these human rights obligations.
Evidence from two studies suggests that grounds-based laws may indirectly contribute to continuation of pregnancy [28, 33]. When grounds-based laws are removed, and first trimester abortion is allowed on request, these studies demonstrated a decrease in fertility, possibly due to a reduction in unplanned births [28, 33]. If, as these studies suggest might be the case, grounds are associated with unwanted continuation of pregnancy, they have clear implications for the right to decide on the number and spacing of children, as well as the right to privacy and to the highest attainable standard of physical and mental health. This is reinforced by the findings from two studies, which suggest that grounds-based laws may contribute to reproductive coercion through the denial of an abortion [18, 24]. This includes people who seek abortion in circumstances where IHRL requires it to be available, namely where the life and health of the pregnant woman or girl is at risk, or where carrying a pregnancy to term would cause her substantial pain or suffering [3]. Denial of abortion in such circumstances has been found to amount to torture, cruel, unusual, and degrading treatment or punishment, including where abortion on the grounds of fatal fetal impairment was unlawful [34, 35].
States have a long-standing obligation in IHRL to ensure that their regulatory choices—in this case grounds-based approaches to abortion—do not force women to resort to unsafe abortion and, if necessary, to review, reform and liberalize laws to ensure this ([3, 36], para 28). Three studies indicate that grounds-based approaches are associated with people availing of unlawful abortion per se [25,26,27], while two indicate an association with self-managed abortion [26, 32]. Self-managed abortion is not necessarily ‘unsafe’, but when availed of outside of the formal legal system and without the availability of appropriate and high-qualify information, medicines (including for pain management), and, where it is desired, support from trained health workers within the health system it can be understood as less safe [37]. Thus, grounds-based approaches engage states’ obligation to review, reform and liberalize their laws to reduce recourse to unsafe abortion ([36], para 28).
Evidence from 15 studies shows that grounds-based approaches contribute to opportunity costs [13,14,15,16,17, 20,21,22,23,24, 26, 29,30,31,32]. These costs are varied and include the need to travel for an abortion [26, 27], increased financial costs, emotional stress and trauma [26, 27] fear or experience of judgement and stigma [15], bureaucratic and costly protracted legal processes [14, 21, 29, 30], increased morbidity, being subjected to ‘nterrogations’ and having one’s rape claim questioned [16], unsafe abortions, and having to carry an unwanted pregnancy or a pregnancy with severe malformations to term [18].
The findings from some of these studies point to an inconsistency in how grounds are interpreted and applied, which sometimes leads to unpredictability and inequity in terms of abortion access and healthcare quality for the abortion seeker [13, 20, 23, 31] and requirements to provide legally-unnecessary documentation or ‘proof’ of fulfilling a ground [13, 17, 19]. One study shows that women who could obtain legal support and advice considered it vital to their ability to navigate the system of abortion provision [22]. In some cases, women who sought abortion based on a recognized ground reported verbal abuse and denial of services [21], and women who had to travel to access abortion sometimes reported reluctance to seek post-abortion care in cases of complications later [32]. The findings from other studies indicate that certain grounds, such as health and rape grounds, are consistently interpreted very restrictively, leading to the denial of abortion [16, 17, 21,22,23,24, 29, 30]. These studies indicate that a grounds-based approach is not sufficient to ensure that the state’s obligation to ensure abortion is lawful and available when continuing with pregnancy would cause substantial pain and suffering is fulfilled ([3], para 4).
five studies suggests that grounds-based approaches have a disproportionate impact on some groups of women [16, 18, 19, 23, 31] and thus undermine the right to equality and non-discrimination which is fundamental to the right to the highest attainable standard of physical and mental health. These studies suggest that in a grounds-based system of abortion law those with fewer resources [19], rural women, and women with lower education [18], as well as those seeking abortion due to rape [16] and on health grounds [23] are relatively less able to access abortion than other women.
Impact of grounds on health professionals
A summary of the findings of grounds-based approaches on health professionals and the application of human rights are presented in Table 3. Evidence identified per study and outcome are presented in Supplementary Tables 1 and 2.
Evidence from five studies suggests that grounds have workload implications for health professionals [13, 18, 19, 24, 25] including difficulties in interpreting and applying the law [24], preparing detailed files for court reviews [18], stress and fear of legal repercussions [25], and frustration with the system when a diagnosis of a non-lethal fetal malformation has been made but abortion is not permitted [18, 19]. Findings from one study suggest that, in order to circumvent obstacles posed by or emanating from grounds-based approaches, referrals may be made to another provider operating in a setting where the ground in question does not preclude access to abortion [14]. One study suggests that where grounds do not permit abortion in situations of diagnosed fetal impairment, health professionals experience this as an imposition on their conscience or ethics [19]. Indeed, in another study the evidence showed that providers perceive grounds-based approaches as an imposition on their conscience or ethics to the extent that they question whether or not they should provide a legal abortion [24]. Findings from one study indicate that grounds-based laws may contribute to stigmatization of abortion provision and healthcare professionals ultimately choosing not to involve themselves in abortion care for this reason [17]. Evidence from five studies suggests that grounds-based laws may contribute to system costs. Indirect contributions to system costs are indicated by continuation of pregnancy and maternal mortality [19, 29, 33]. Direct contributions to system costs include the imposition of costs on court systems, increased workloads forhealthcare professionals [18], and delays to care for pregnant women with severe health conditions [27].
Evidence of the impact of grounds on health professionals points not only to their conditions of work but also to the implications of grounds for the health system and, thus, for the right to the highest attainable standard of physical and mental health. That right obliges states to ensure that health-care facilities, goods, and services are available, accessible, acceptable and of good quality ([38], paras 4, 12).
Overall, the evidence from these studies suggests that grounds-based approaches to abortion regulation undermine the right to health by impacting on health workers and the health system so as to make sexual and reproductive healthcare less available, accessible, and acceptable and to lower its quality.
Discussion
Making abortion available based on grounds, sometimes after a limited period during which it is available without restriction as to reason, is a common approach to law and policy on abortion. To illustrate, as of February 2019 there were only 16 jurisdictions that prohibited abortion in all circumstances, and seven more where laws prohibited unlawful abortion but failed to specify expressly the grounds for lawful abortion [1]. States that have recently transitioned from near-total bans on abortion to some or wide legal availability have tended to adopt a grounds-based approach [39,40,41]. In addition, several constitutional and other courts have recently intervened to determine the constitutionality of abortion law in specified circumstances [42,43,44,45,46,47,48,49]. It is clear that using grounds as a mode of designing abortion provision is persistent. However, the evidence presented in this review suggests that this approach is suboptimal from a rights-based perspective. While modes of providing abortion care may vary as a pregnancy develops, whether and if so how abortion is provided should not be determined by legally prescribed grounds but by the preferences of the pregnant person and evidence-based clinical and service delivery protocols [9].
The evidence from this review shows that grounds-based approaches implicate states’ obligation to ensure that abortion is lawfully available where carrying a pregnancy to term would cause a pregnant woman substantial pain or suffering, where there is a risk to life or health, where pregnancy is a result of rape or incest, or where the pregnancy is not viable ([3], para 4). This is because grounds-based approaches to abortion provision are per se restrictive and are commonly subject to narrow interpretation, limitation and burdensome procedures so that ‘qualification’ for abortion under such grounds is very difficult to establish. As this can lead to women having recourse to less safe or unsafe abortions, grounds-based approaches engage states’ obligation to take steps, including revising their laws, to ensure women do not have to undergo unsafe abortion ([3, 4], para 6), to reduce maternal morbidity and mortality, and to effectively protect women and girls from the physical and mental risks associated with unsafe abortions. The evidence in this review points towards allowing abortion on request as the most effective approach to ensuring that abortion is available in the circumstances required by IHRL. In addition to being an effective mode of satisfying pregnant people’s rights, this would also mean that women are not required—and do not feel obliged—to provide reasons or justifications for their decision to end their pregnancies. Instead of defining only certain circumstances where abortion is permitted and thus, implicitly, justifiable, and the person seeking it deserving of abortion care, the provision of abortion without restriction as to reason would center the pregnant person’s reproductive autonomy and support her in giving effect to her assessment of what is right for her, regardless of circumstances. This is consistent with established frameworks for quality of care as well as with IHRL. Indeed, the WHO has now recommended against grounds-based approaches and recommended that abortion be made available on the request of the pregnant person [9].
Limitations
This review has limitations. While the studies relate to 13 settings, this is nevertheless limited when compared to the number of jurisdictions that take a grounds-based approach to abortion [1]. This review also only contains manuscripts published in English. Further research on the impact of grounds in a wider range of settings would be valuable.
The realization of human rights applicable to abortion-related interventions is not a research area that readily lends itself to randomized controlled trials or comparative observational studies; rather, studies are often conducted without comparisons. While this may be considered a limitation from a standard methodological perspective for systematic reviews, it does not limit the ability to identify the human rights law implications of grounds-based approaches. Thus, while standard tools for assessing risk of bias or quality, including GRADE [50], were unsuitable, given the objective of fully integrating human rights implications into our understanding of the effects of grounds as a regulatory intervention, it was appropriate to engage with a wide variety of sources. Finally, and consistent with the methodological approach pursued [6], this review applies international, rather than regional or domestic, human rights law to develop a general understanding of the rights-related implications of grounds. The applicability of any individual human rights standard in a specific setting will depend on factors including the state’s ratification of relevant human rights instruments and their status in domestic law ([9], p. 7).
Conclusions
The evidence from this review shows that grounds-based approaches to abortion limit access to abortion both because they exclude some women due to non-satisfaction of grounds and because they can operate in a way that makes availability and accessibility narrower in practice due to the chilling effects of continued criminalization, the burdens on providers, and the space they leave for conservative and limiting interpretation. Combining the evidence from the review of studies with evidence of applicable human rights standards indicates that grounds-based approaches result in violations of human rights. This points to the regulatory and human rights value of ensuring access to abortion on request of the pregnant person as a rights compliant, autonomy-based, and effective step in putting in place a supportive law and policy framework to support an enabling environment for quality abortion care.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- IHRL:
-
International Human Rights Law
- WHO:
-
World Health Organization
References
Lavelanet A, Johnson BR, Ganatra B. Global abortion policies database: a descriptive analysis of the regulatory and policy environment related to abortion. Best Pract Res Clin Obstet Gynaecol. 2020;62:25–35.
Lavelanet A, Schlitt S, Jonson B, Ganatra B. Global abortion policies database: a descriptive analysis of the legal categories of lawful abortion. BMC Int Health Hum Rights. 2018;18(44):1–10. https://doi.org/10.1186/s12914-018-0183-1.
Human Rights Committee, General comment no.36; article 6 right to life. 2018 (UN Doc CCPR/C/GC/36).
Human Rights Committee, General comment no. 28: Equality of rights between men and women) (article 3) (2000) (UN Doc. CCPR/C/21/Rev.1/Add.10).
Committee on the Rights of the Child, General comment no. 4: Adolescent health and development in the context of the Convention on the Rights of the Child. 2003) (UN Doc. CRC/GC/2003/4).
de Londras F, Cleeve A, Rodriguez M, Lavelanet A. Integrating rights and evidence: a technical advance in abortion guideline development. BMJ Glob Health. 2021;6:e004141.
Petticrew M, Knai C, Thomas J, et al. Implications of a complexity perspective for systematic reviews and guideline development in health decision making. BMJ Glob Health. 2019;4:e000899. https://doi.org/10.1136/bmjgh-2018-000899.
Thomson HJ, Thomas S. The effect direction plot: visual display of non-standardised effects across multiple outcome domains. Res Synth Methods. 2013;4(95):101. https://doi.org/10.1002/jrsm.1060pmid.
World Health Organization, Abortion care guideline. 2022.
Burris S, Ghorashi A, Foster Cloud L, Rebouché R, Skuster P, Lavelanet A. Identifying data for the empirical assessment of law (IDEAL): a realist approach to research gaps on the health effects of abortion law. BMJ Glob Health. 2021;6:e005120. https://doi.org/10.1136/bmjgh-2021-005120.
World Health Organization. Safe abortion: technical and policy guidance for health systems. 2nd ed; 2012.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71. For more information, visit: http://www.prismastatement.org/.
Ramos S, Romero M, Ramón MA. Health care providers’ opinions on abortion: a study for the implementation of the legal abortion public policy in the province of Santa Fe, Argentina. Reprod Health. 2014;11:72.
Black KI, Douglas H, de Costa C. Women’s access to abortion after 20 weeks’ gestation for fetal chromosomal abnormalities: views and experiences of doctors in New South Wales and Queensland. Austr N Z J Obstet Gynaecol. 2015;55:144.
LaRoche KJ, Wynn LL, Foster AM. We have to make sure you meet certain criteria’: exploring patient experiences of the criminalisation of abortion in Australia. Public Health Res Pract. 2021;31(3):30342011. https://doi.org/10.17061/phrp30342011.
Diniz D, Madeiro A, Rosas C. Conscientious objection, barriers, and abortion in the case of rape: a study among physicians in Brazil. Reprod Health Matters. 2014;22(43):141–8.
Madeiro AP, Diniz D. Legal abortion in Brazil—a national study. Cien Saude Colet. 2016;21(2):563–72. https://doi.org/10.1590/1413-81232015212.10352015.
Mirlesse V, Ville I. The uses of ultrasonography in relation to foetal malformations in Rio de Janeiro, Brazil. Soc Sci Med. 2013;87:168–75.
Casas L, Vivaldi L. Pregnancies and fetal anomalies incompatible with life in Chile: arguments and experiences in advocating for legal reform. Health Hum Rights J. 2017;19(1):95–108.
Maira G, Casas L, Vivaldi L. Abortion in Chile: the long road to legalization and its slow implementation. Health Hum Rights J. 2019;21(2):121–32.
Amado ED, Calderón García MC, Cristancho KR, et al. Obstacles and challenges following the partial decriminalisation of abortion in Colombia. Reprod Health Matters. 2010;18(36):118–26.
DePiñeres T, Raifman S, Mora M, et al. ‘I felt the world crash down on me’: Women’s experiences of being denied legal abortion in Colombia. Reprod Health. 2017;14:133.
Küng SA, Darney BG, Saavedra-Avendaño B, et al. Access to abortion under the health exception: a comparative analysis in three countries. Reprod Health. 2018;15:107.
McLean E, Desalegn DN, Blystad A, Miljeteig I. When the law makes doors slightly open: ethical dilemmas among abortion service providers in Addis Ababa, Ethiopia. BMC Med Ethics. 2019;20:60.
Payne CM, Precourt Debbink M, Steele EA, et al. Why women are dying from unsafe abortion: narratives of Ghanaian abortion providers. Afr J Reprod Health. 2013;17(2):118–28.
Aiken ARA, Johnson DM, Broussard K, Padron E. Experiences of women in Ireland who accessed abortion by travelling abroad or by using abortion medication at home: a qualitative study. BMJ Sex Reprod Health. 2018;44:181–6.
Aitken K, Patek P, Murphy ME. The opinions and experiences of Irish obstetric and gynaecology trainee doctors in relation to abortion services in Ireland. J Med Ethics. 2017;43:778–83.
Clarke D and Mühlrad H, “The impact of abortion legalization on fertility and maternal mortality: New Evidence from Mexico” (2016) CINCH series #2016/02.
Påfs J, Rulisa S, Klingberg-Allvin M, et al. Implementing the liberalized abortion law in Kigali, Rwanda: ambiguities of rights and responsibiltiies among health care providers. Midwifery. 2020;80:102568.
Sahin Hodoglugil NN, Ngabo F, Ortego J, et al. Making abortion safer in Rwanda. Afr J Reprod Health. 2017;21(1):82–92.
Arnott G, Sheehy G, Chinthakanan O, Foster A. Exploring legal restrictions, regulatory reform, and geographic disparities in abortion access in Thailand. Health Hum Rights J. 2017;19(1):187–95.
Aiken ARA, Padron E, Broussard K, Johnson D. The impact of Northern Ireland’s abortion laws on women’s abortion decision-making and experiences. BMJ Sex Reprod Health. 2019;45:3–9.
Antón J-I, Ferre Z, Triunfo P. The impact of the legalisation of abortion on birth outcomes in Uruguay. Health Econ. 2018;27:1103–19.
HRC, Amanda Mellet v Ireland. 2013. UN Doc. CCPR/C/116/D/2324/2013.
HRC, Siobhan Whelan v Ireland. 2014. UN Doc CCPR/C/119/D/2425/201.
CESCR. General comment no. 22 on the right to sexual and reproductive health (article 12 of the international covenant on economic, Social and Cultural Rights). 2016. UN Doc. E/C/12/GC/22.
Ganatra B, et al. Global, regional and subregional classification of abortions by safety, 2010–14: estimates from a Bayesian hierarchical model. Lancet. 2017;390(10110):2372–81.
Committee on Economic, Social and Cultural Rights, General comment no. 14: The right to the highest attainable standard of health (article 12 of the International Covenant on Economic, Social and Cultural Rights). 2000. UN Doc. E/C.12/2000/4.
Health (Regulation of Termination of Pregnancy) Act 2018 (Ireland).
Crimes (Amendment) Act 2019 (Gibraltar).
Proclamation No. 414/2004 (2005) (Ethiopia).
National Supreme Court of Justice of Argentina. Corte Suprema de Justicia de la Nación, F, A. L. s/Medida Autosatisfactiva, Expediente Letra “F”, N° 259, Libro XLVI. 2012.
Sentencia C-355/06, Part VI, Constitutional Court of Colombia. 2006.
STC Rol N° 3729(3751)-17 CPT, Constitutional Court of Chile. 2017.
Claim of noncompliance with fundamental Precept no.54. Judge-rapporteur: justice Marco Aurélio. Vote: justice Rosa Weber. Brasília: Supreme Court of Brazil, 2013.
The matter of an application by the Northern Ireland human rights Commission for Judicial Review (Northern Ireland). 2018, UKSC 27.
R (On the application of A and B) v SoS for Health [2017] UKSC 41.
Maneula and family v El Salvador, Inter-American Court of Human Rights, Case 13.069. 2018.
Constitutional Tribunal of Poland, decision K 1/20, 2020.
Alonso-Coello P, Schünemann HJ, Moberg J, et al. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1. Introduction. BMJ. 2016;353:i2016.
Acknowledgements
We record thanks to Alana Farrell for assistance in final preparation of the manuscript.
Funding
This work was supported by the UNDP-UNFPA-UNICEF-WHO-World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), a cosponsored programme executed by the World Health Organization (WHO). Professor de Londras also acknowledges the support of the Leverhulme Trust through the Philip Leverhulme Prize.
Author information
Authors and Affiliations
Contributions
AL and FdL developed the PICOs and search strategies. AC and FdL did the initial searches. AL, AC, MR and FdL reviewed and finalised data extraction and quality. FdL did the initial manuscript draft. AL prepared the tables and figures. All authors reviewed, finalised and approved the submitted text.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Suppl Table 1.
Evidence table: Impact on the intervention on abortion seekers. Supple Table 2. Evidence Table: The impact of the intervention on health professionals.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
de Londras, F., Cleeve, A., Rodriguez, M.I. et al. The impact of ‘grounds’ on abortion-related outcomes: a synthesis of legal and health evidence. BMC Public Health 22, 936 (2022). https://doi.org/10.1186/s12889-022-13247-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-13247-0